Q3 Financial Results & �ASH Abstracts Investor Webcast November 5, 2024

Beam conference call participants Beam’s Sickle Cell Disease Strategy Q3 Business Update Introduction ASH Abstract: ESCAPE Preclinical Data ASH Abstracts: BEAM-101 Clinical Data Mr. Evans John Evans�Chief Executive Officer Holly Manning�VP Investor Relations & External Communications Giuseppe Ciaramella, Ph.D. �President Amy Simon, M.D. �Chief Medical Officer Closing Remarks Mr. Evans Q&A Mr. Evans, Dr. Simon, Dr. Ciaramella TOPIC PARTICIPANT
Cautionary note regarding forward-looking statements This presentation contains forward-looking statements within the meaning of the Private Securities Litigation Reform Act of 1995. Such forward-looking statements include statements regarding: the therapeutic applications and potential of our technology, including with respect to SCD, T-ALL/T-LL, AATD, GSD1a, and ESCAPE; our plans, and anticipated timing, to advance our programs; the clinical trial designs and expectations for BEAM-101, BEAM-201, BEAM-301, BEAM-302 and ESCAPE; our potential presentations at the ASH annual meeting; our current expectations and anticipated results of operations, including our expected use of capital; the sufficiency of our capital resources to fund operating expenses and capital expenditure requirements and the period in which such resources are expected to be available; and the therapeutic applications and potential of our technology, including our potential to develop life-long, curative, precision genetic medicines for patients through base editing, including potential safety advantages, all of which are subject to known and unknown important risks, uncertainties and other factors that may cause our actual results, performance or achievements, market trends, or industry results to differ materially from those expressed or implied by such forward-looking statements. Therefore, any statements contained herein that are not statements of historical fact may be forward-looking statements and should be evaluated as such. Without limiting the foregoing, the words "anticipate," "expect," "suggest," "plan," "vision," "believe," "intend," "project," "forecast," "estimates," "targets," “strategy,” “possibilities,” “promise,” "projections," "potential," "should," "could," "would," "may," "might," "will," and the negative thereof and similar words and expressions are intended to identify forward-looking statements. Each forward-looking statement is subject to important risks and uncertainties that could cause actual results to differ materially from those expressed or implied in such statement, including, without limitation, risks and uncertainties related to: our ability to develop, obtain regulatory approval for, and commercialize our product candidates, which may take longer or cost more than planned; our ability to raise additional funding, which may not be available; our ability to obtain, maintain and enforce patent and other intellectual property protection for our product candidates; the uncertainty that our product candidates will receive regulatory approval necessary to initiate human clinical trials; that preclinical testing of our product candidates and preliminary or interim data from preclinical studies and clinical trials may not be predictive of the results or success of ongoing or later clinical trials; that initiation and enrollment of our clinical trials may take longer than expected; that our product candidates or the delivery modalities we rely on to administer them may cause serious adverse events; that our product candidates may experience manufacturing or supply interruptions or failures; risks related to competitive products; and the other risks and uncertainties identified under the headings "Risk Factors Summary" and "Risk Factors" and elsewhere in our annual report on Form 10-K for the year ended December 31, 2023, our quarterly reports on Form 10-Q, and in any subsequent filings with the Securities and Exchange Commission (the "SEC") which are available on the SEC's website at www.sec.gov. Additional information will be made available by our annual and quarterly reports and other filings that we make from time to time with the SEC. These forward-looking statements speak only as of the date of this presentation. Factors or events that could cause our actual results to differ may emerge from time to time, and it is not possible for us to predict all of them. We undertake no obligation to update any forward-looking statement, whether as a result of new information, future developments or otherwise, except as may be required by applicable law.
OUR VISION IS TO PROVIDE LIFE-LONG CURES �for patients suffering from serious diseases POTENTIAL FOR �one-time, curative therapies GENE EDITING FOR �rare and common diseases PLATFORM FOR �rapidly programmable precision medicines
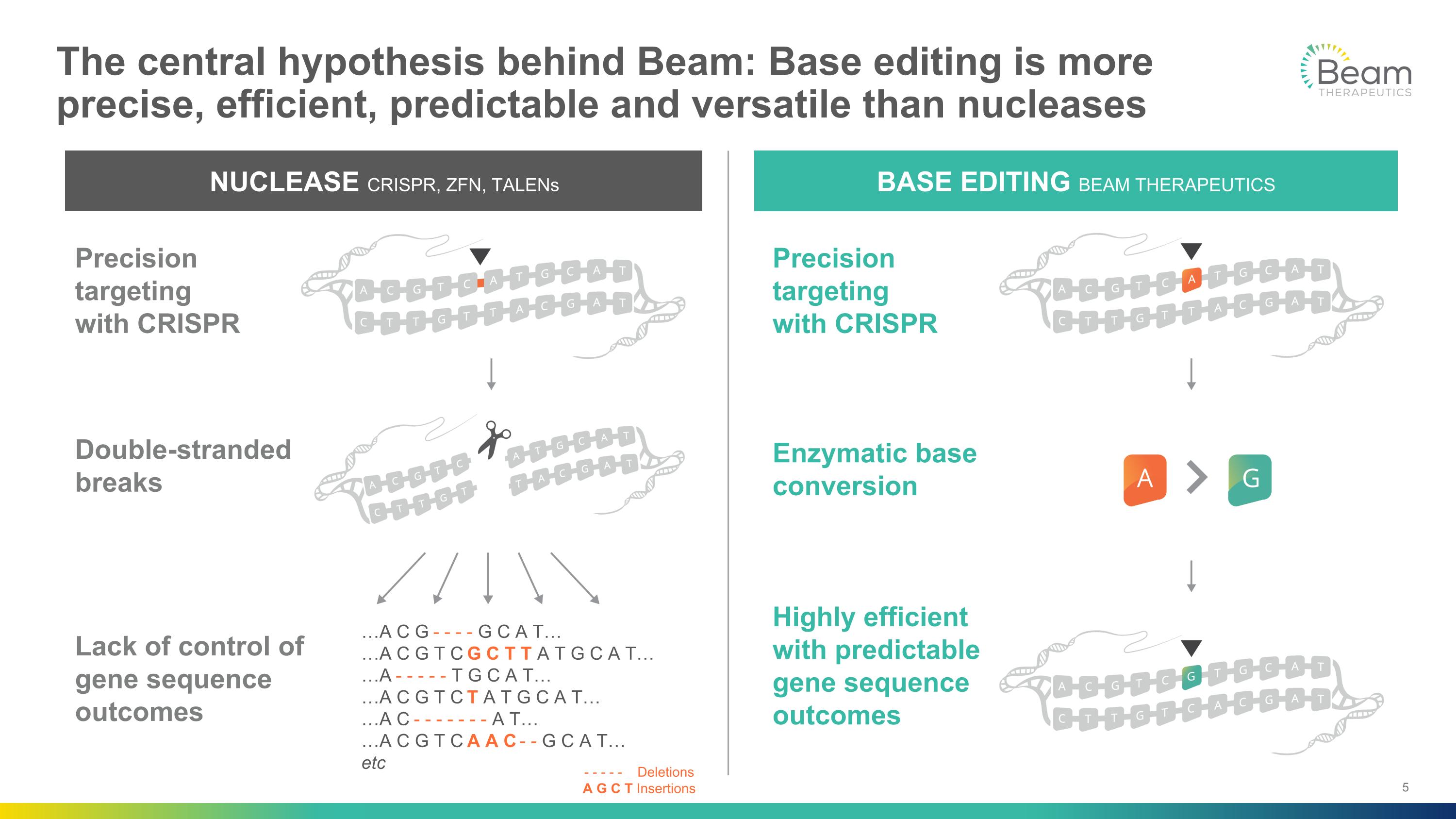
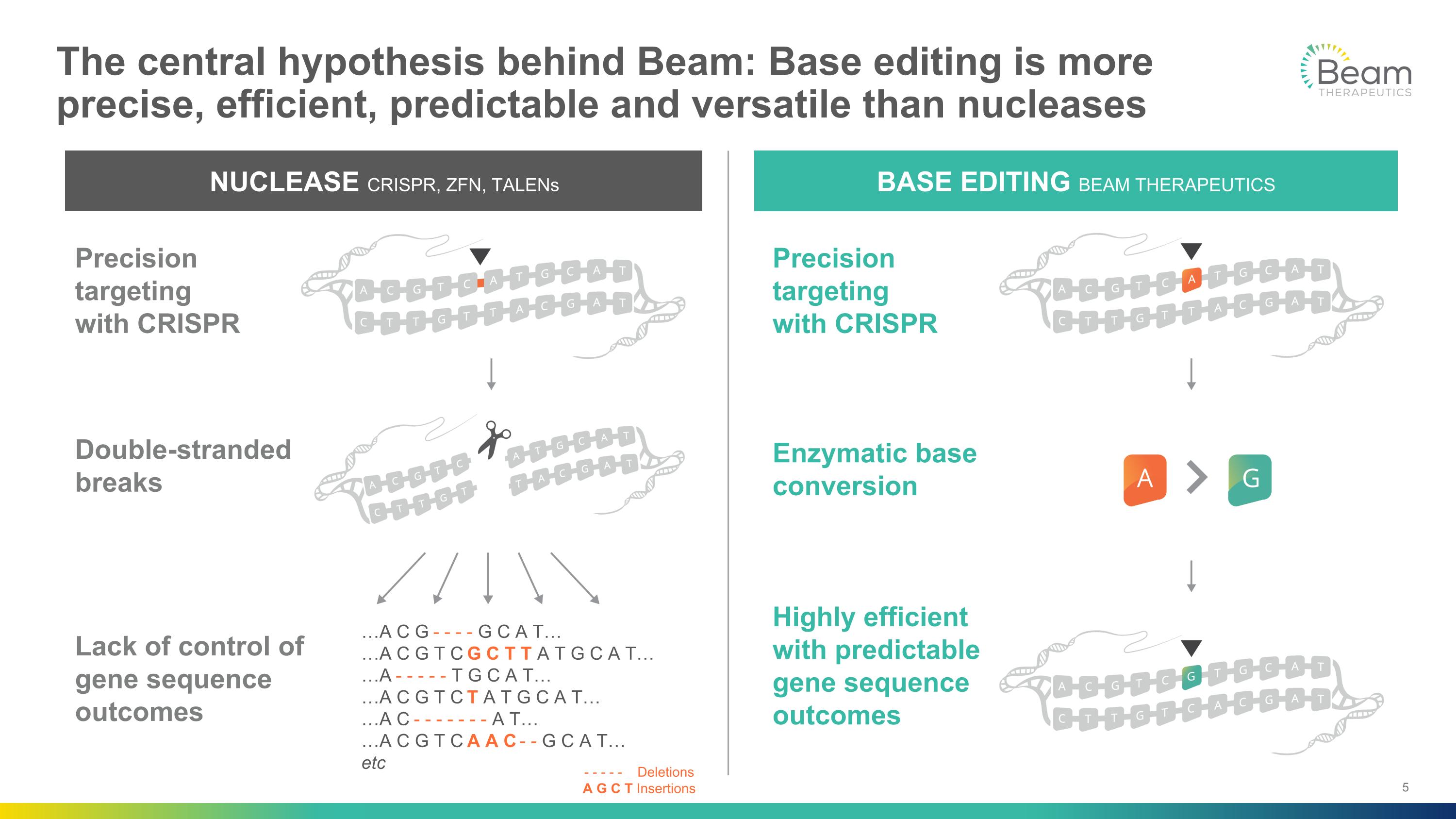
The central hypothesis behind Beam: Base editing is more precise, efficient, predictable and versatile than nucleases NUCLEASE CRISPR, ZFN, TALENs Double-stranded breaks Lack of control of gene sequence outcomes Precision targeting�with CRISPR BASE EDITING BEAM THERAPEUTICS Enzymatic base conversion Highly efficient with predictable gene sequence outcomes Precision targeting�with CRISPR …A C G - - - - G C A T… …A C G T C G C T T A T G C A T… …A - - - - - T G C A T… …A C G T C T A T G C A T… …A C - - - - - - - A T… …A C G T C A A C - - G C A T… etc - - - - - Deletions A G C T Insertions

Two platforms with potential to create transformative therapies and significant value creation Hematology Liver Genetic Diseases Best-in-class potential for BEAM-101 for sickle cell disease (SCD) Increased probability of technical success for ex vivo gene editing and fetal hemoglobin (HbF) upregulation Validated FDA regulatory pathway ESCAPE has potential to eliminate chemotherapy from transplant, expanding reach of base editing to more patients Platform for future hematology pipeline Best-in-class potential for BEAM-302 for alpha-1 antitrypsin deficiency (AATD) Increased probability of technical success for�in vivo lipid-nanoparticle (LNP) gene editing in liver Potential for rapid clinical proof of concept Clinical-stage AATD program with potential to be a one-time treatment that benefits both lung and liver disease Platform for future liver-targeted pipeline Initial data today Data expected in 2025

Significant execution momentum in Q3 across our priority hematology and liver genetic disease programs Hematology Liver Genetic Diseases First cohort dosing completed in the Phase 1/2 trial of BEAM-302 in AATD IND approved by FDA and site activation activities underway for BEAM-301 Phase 1/2 study in glycogen storage disease 1a (GSD1a) 35 patients enrolled and 8 patients dosed in BEACON Phase 1/2 trial of BEAM-101 in SCD Development candidate nominated for ESCAPE technology in SCD: BEAM-103 (anti-CD117 mAb) BEAM-104 (CD34 cells with a CD117 edit and HBG1/2 edit) $925.8M in cash with expected operating runway into 2027 (excluding commercialization expenses for BEAM-101)
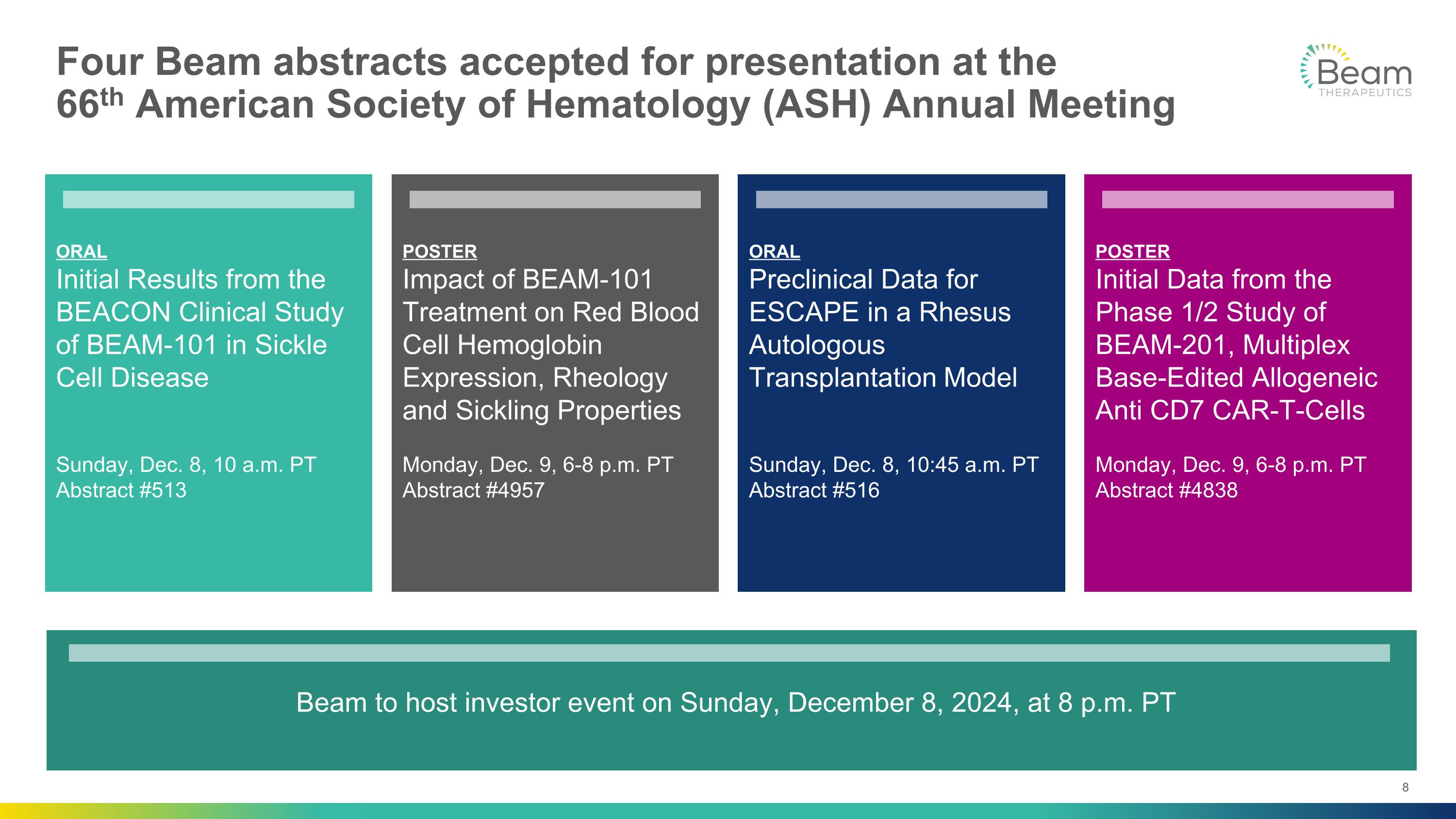
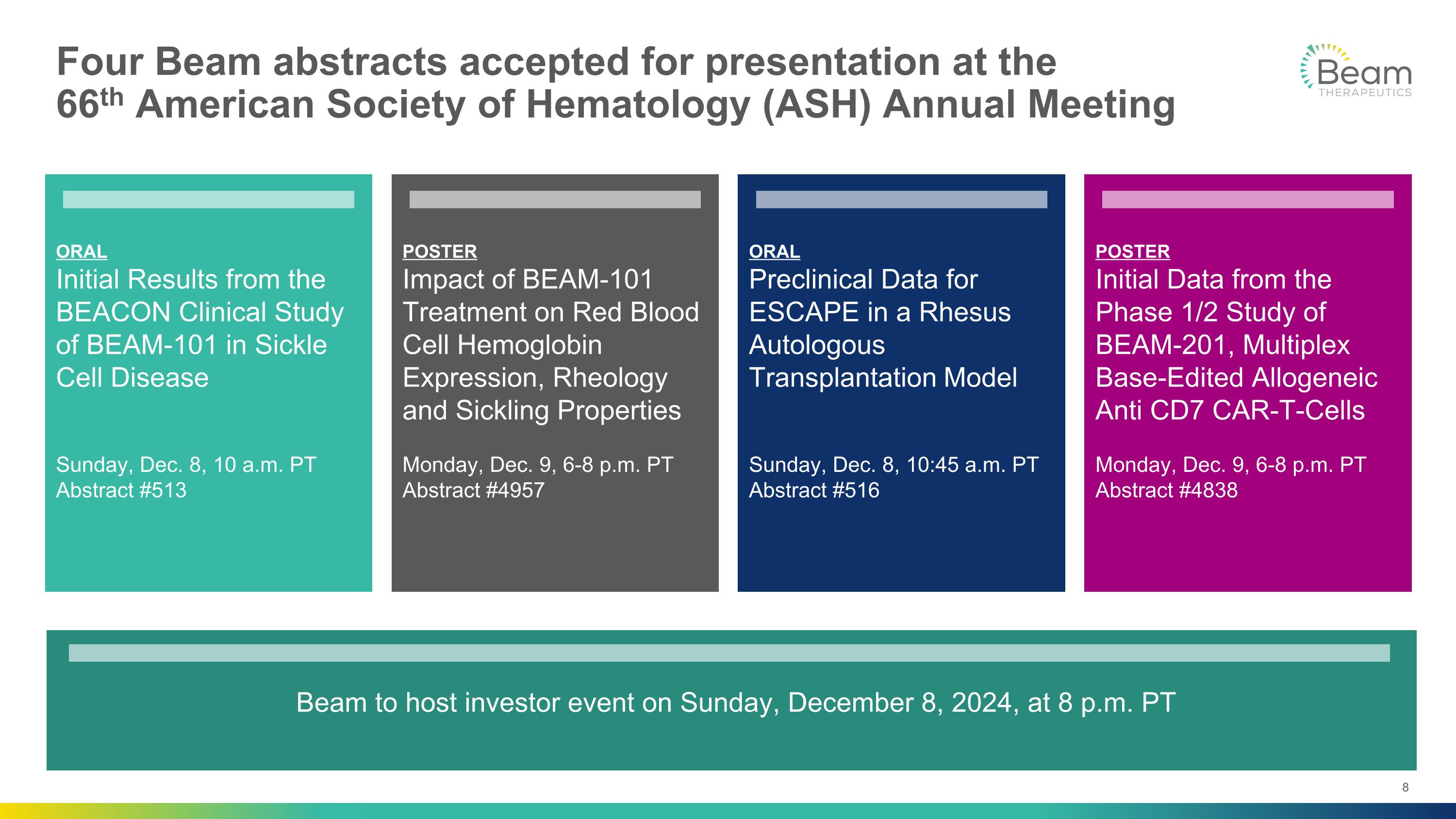
ORAL Initial Results from the BEACON Clinical Study of BEAM-101 in Sickle Cell Disease Sunday, Dec. 8, 10 a.m. PT Abstract #513 ORAL Preclinical Data for ESCAPE in a Rhesus Autologous Transplantation Model Sunday, Dec. 8, 10:45 a.m. PT Abstract #516 POSTER Initial Data from the Phase 1/2 Study of BEAM-201, Multiplex Base-Edited Allogeneic Anti CD7 CAR-T-Cells Monday, Dec. 9, 6-8 p.m. PT Abstract #4838 POSTER Impact of BEAM-101 Treatment on Red Blood Cell Hemoglobin Expression, Rheology and Sickling Properties Monday, Dec. 9, 6-8 p.m. PT Abstract #4957 Four Beam abstracts accepted for presentation at the �66th American Society of Hematology (ASH) Annual Meeting Beam to host investor event on Sunday, December 8, 2024, at 8 p.m. PT

What if we could develop better one-time therapies for people living with SCD? SICKLE CELL DISEASE
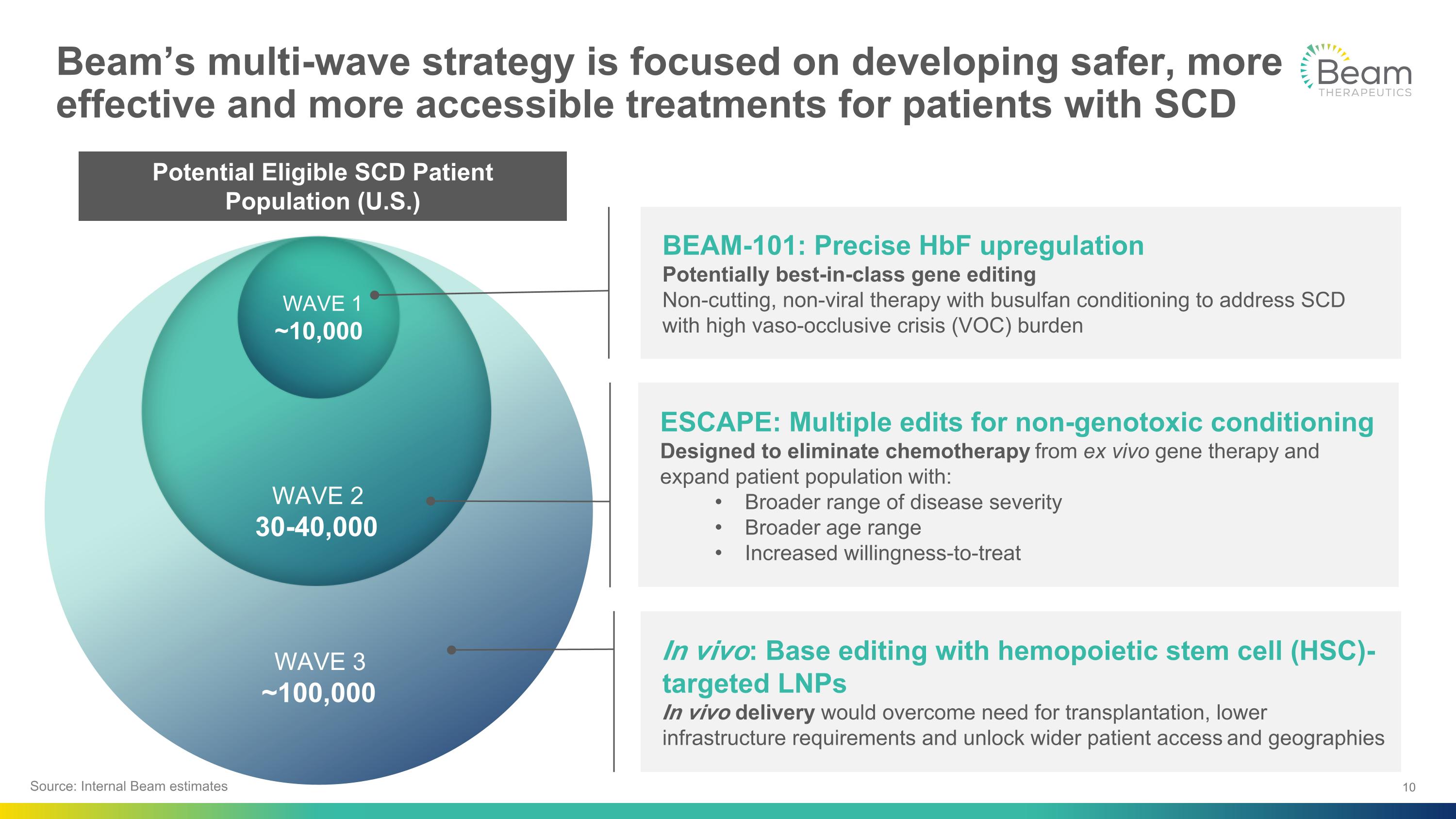
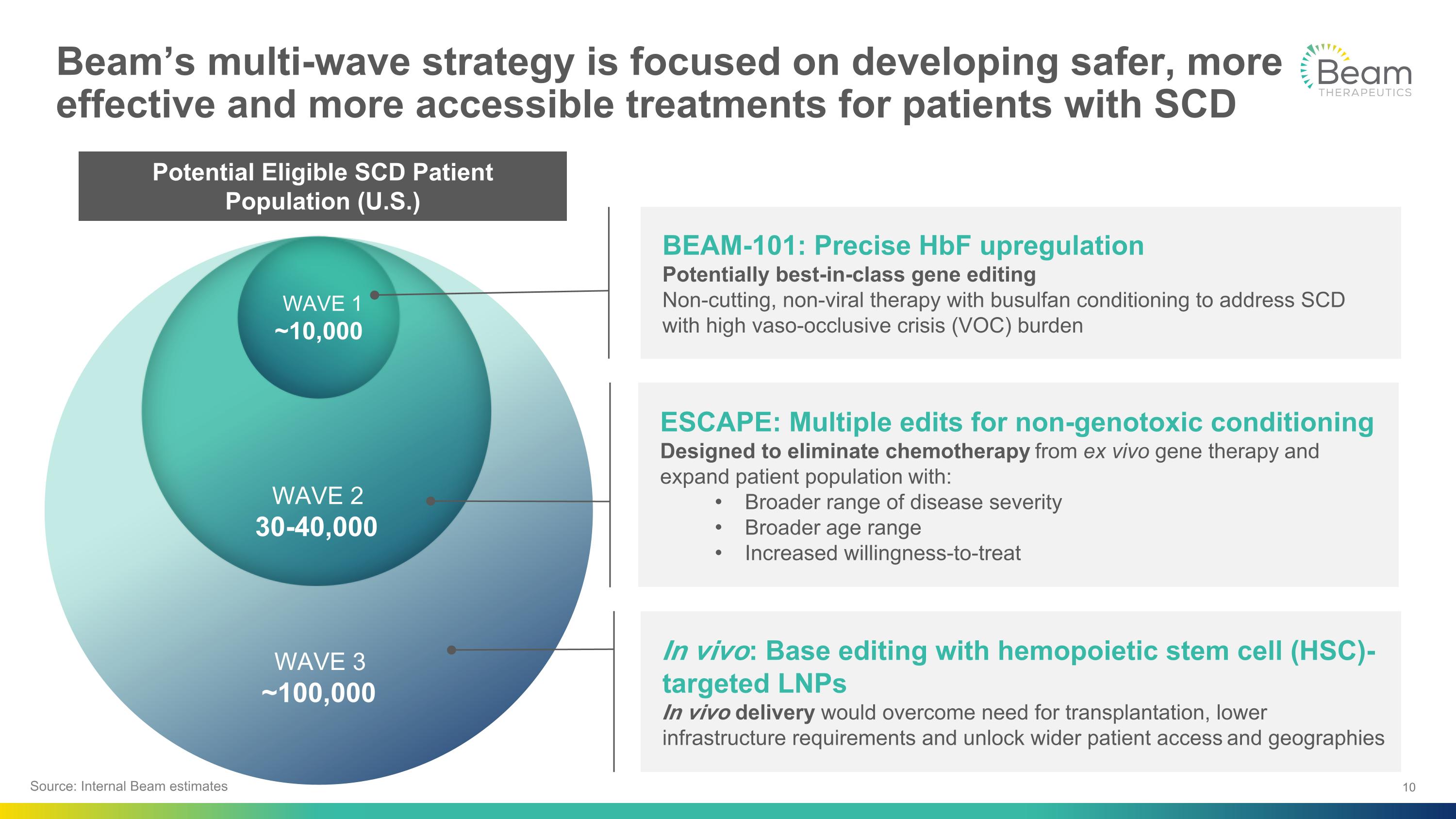
WAVE 3 ~100,000 Beam’s multi-wave strategy is focused on developing safer, more effective and more accessible treatments for patients with SCD WAVE 2 30-40,000 WAVE 1 ~10,000 ESCAPE: Multiple edits for non-genotoxic conditioning Designed to eliminate chemotherapy from ex vivo gene therapy and expand patient population with: Broader range of disease severity Broader age range Increased willingness-to-treat BEAM-101: Precise HbF upregulation Potentially best-in-class gene editing �Non-cutting, non-viral therapy with busulfan conditioning to address SCD with high vaso-occlusive crisis (VOC) burden In vivo: Base editing with hemopoietic stem cell (HSC)-targeted LNPs In vivo delivery would overcome need for transplantation, lower infrastructure requirements and unlock wider patient access and geographies Source: Internal Beam estimates Potential Eligible SCD Patient Population (U.S.)

WAVE 3 ~100,000 Beam’s multi-wave strategy is focused on developing safer, more effective and more accessible treatments for patients with SCD WAVE 2 30-40,000 ESCAPE: Multiple edits for non-genotoxic conditioning Designed to eliminate chemotherapy from ex vivo gene therapy and expand patient population with: Broader range of disease severity Broader age range Increased willingness-to-treat In vivo: Base editing with HSC-targeted LNPs In vivo delivery would overcome need for transplantation, lower infrastructure requirements and unlock wider patient access and geographies Potential Eligible SCD Patient Population (U.S.) Source: Internal Beam estimates WAVE 1 ~10,000 BEAM-101: Precise HbF upregulation Potentially best-in-class gene editing �Non-cutting, non-viral therapy with busulfan conditioning to address SCD with high vaso-occlusive crisis (VOC) burden

BEAM-101: Designed to be best-in-class genetic�medicine for sickle cell disease BEAM-101 Potential SCD Patient HBB HBG1 HBG2 HBB HBG1 HBG2 Mutated hemoglobin gene (HBB) Direct reactivation of fetal hemoglobin (HbF) genes Hemoglobin genes SCD Unmet Need Sickle hemoglobin (HbS) polymerization is root cause of sickle cell pathophysiology Affects millions of people worldwide and ~100K in U.S. Median survival in the U.S. is ≥20 years shorter Current Available Treatments Disease-modifying therapies do not prevent organ dysfunction and require ongoing treatment Recently approved gene therapies reduce VOCs but residual HbS >50% suggests room for improvement Hemoglobin expression Expression of sickle-causing hemoglobin HbF expressed and �HbS decreased HbS HbF RBCs form and function normally RBCs sickle and polymerize with hypoxia Impact on red blood cells (RBCs) CDC Data & Statistics; Lancet Haematol 2023; 10: e585–99; DeBaun et al. Blood. 2019 Feb 7; 133(6):615-617
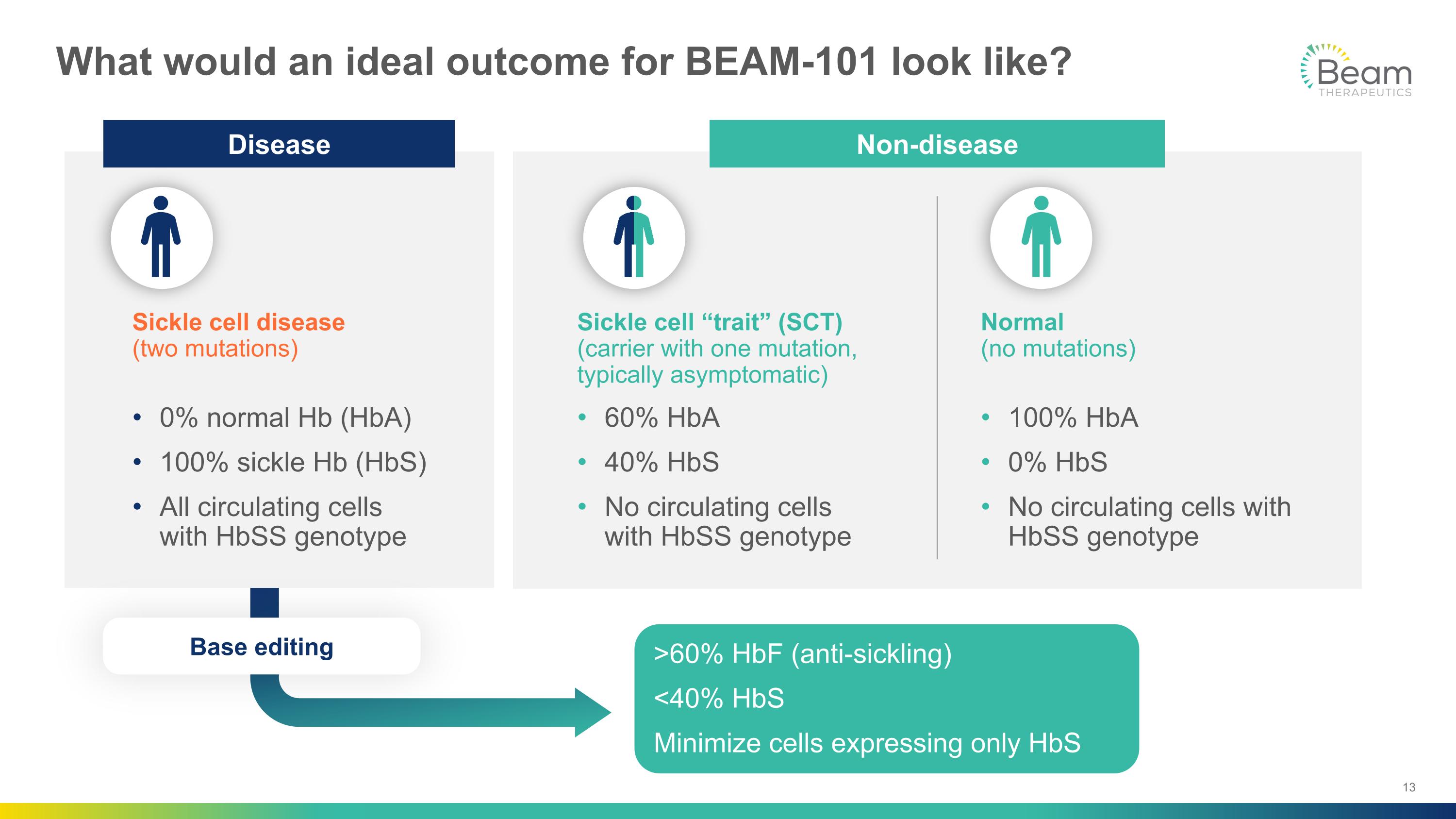
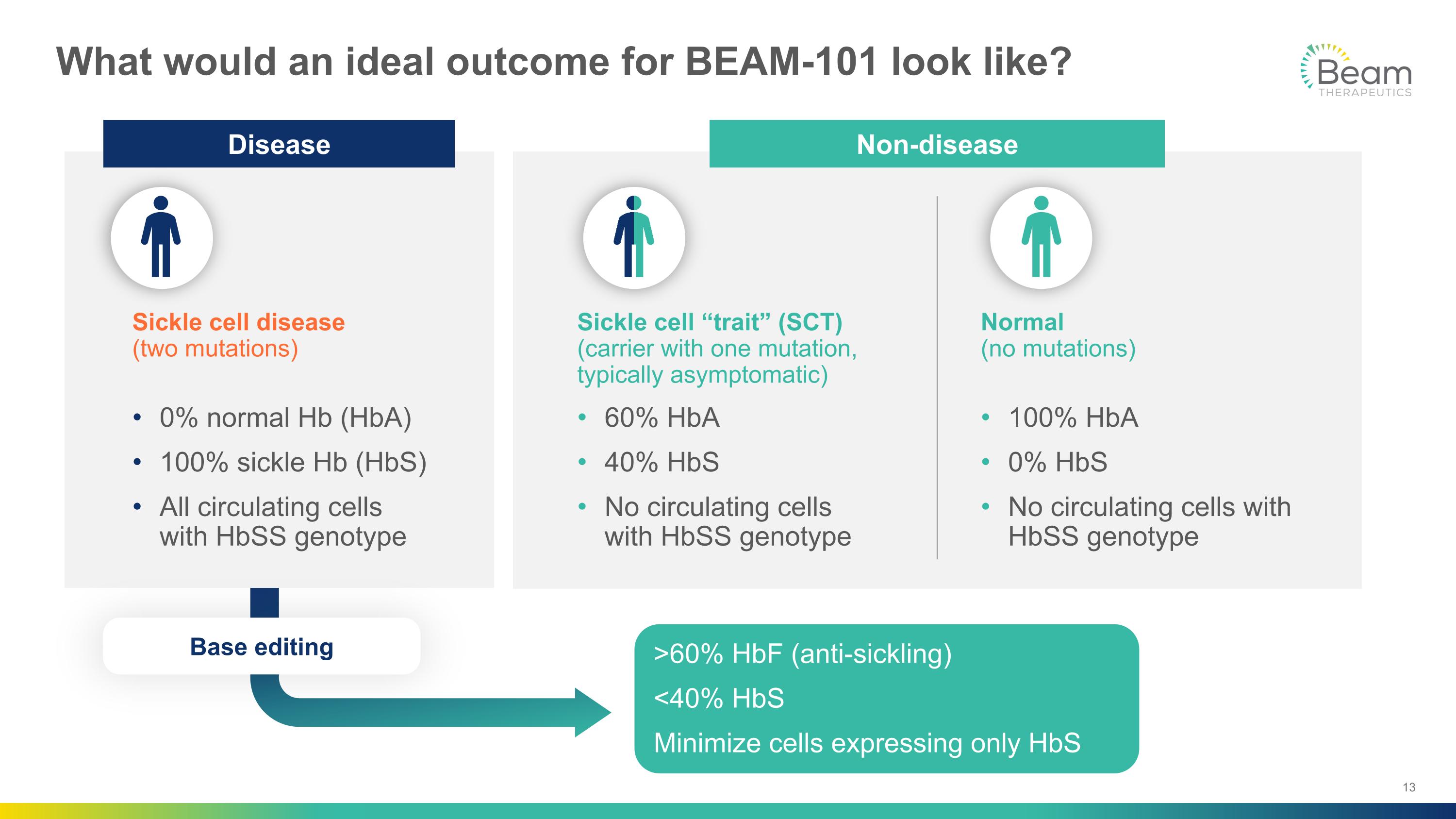
What would an ideal outcome for BEAM-101 look like? Sickle cell “trait” (SCT)�(carrier with one mutation, typically asymptomatic) 60% HbA 40% HbS No circulating cells �with HbSS genotype Normal �(no mutations) 100% HbA 0% HbS No circulating cells with HbSS genotype Sickle cell disease�(two mutations) 0% normal Hb (HbA) 100% sickle Hb (HbS) All circulating cells �with HbSS genotype >60% HbF (anti-sickling) <40% HbS Minimize cells expressing only HbS Non-disease Disease Base editing
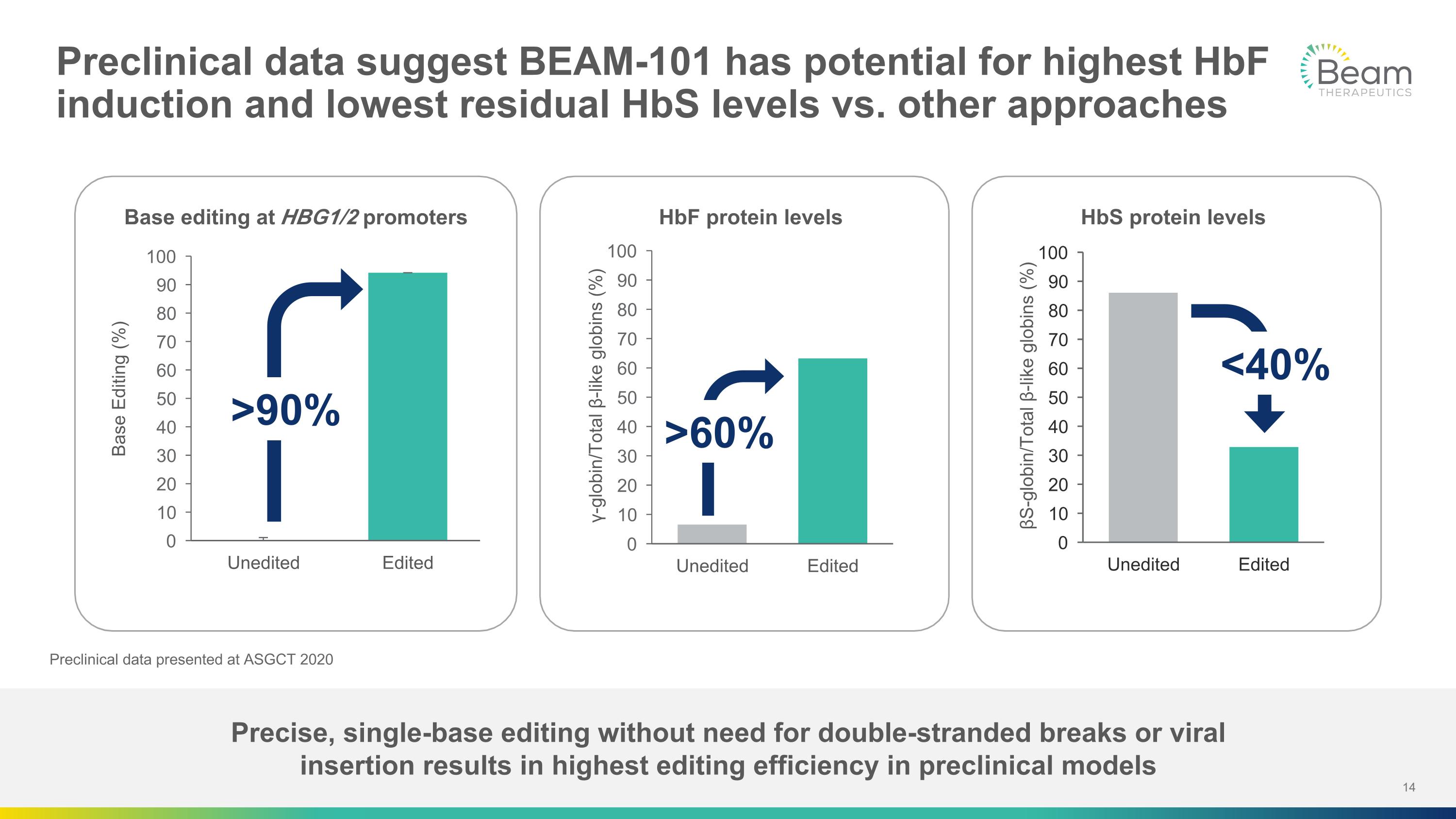
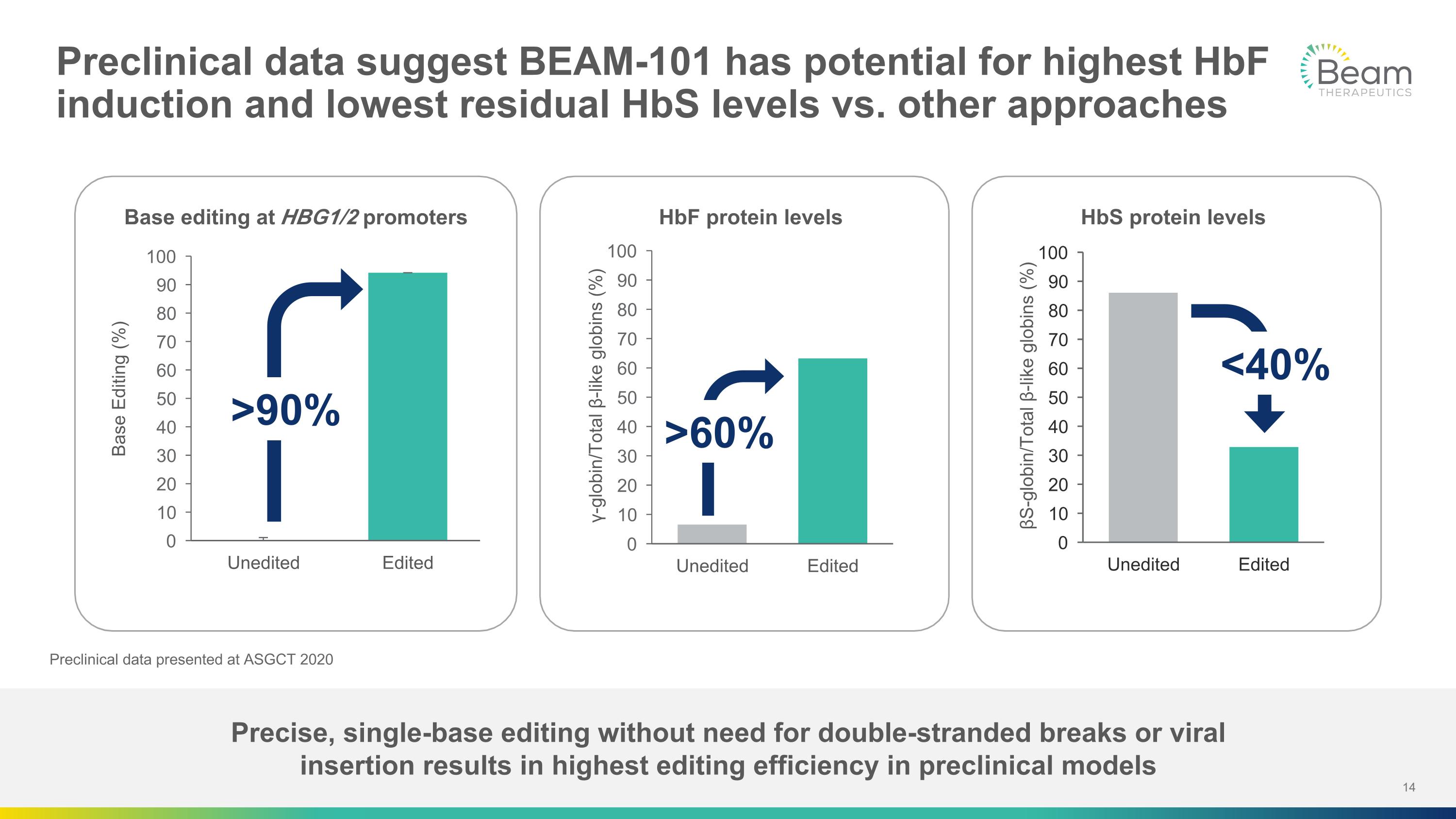
Precise, single-base editing without need for double-stranded breaks or viral �insertion results in highest editing efficiency in preclinical models Preclinical data suggest BEAM-101 has potential for highest HbF induction and lowest residual HbS levels vs. other approaches Preclinical data presented at ASGCT 2020 Base editing at HBG1/2 promoters HbF protein levels HbS protein levels >90% >60% <40%
BEAM-101 Phase 1 Clinical Data AMY SIMON, M.D., CHIEF MEDICAL OFFICER
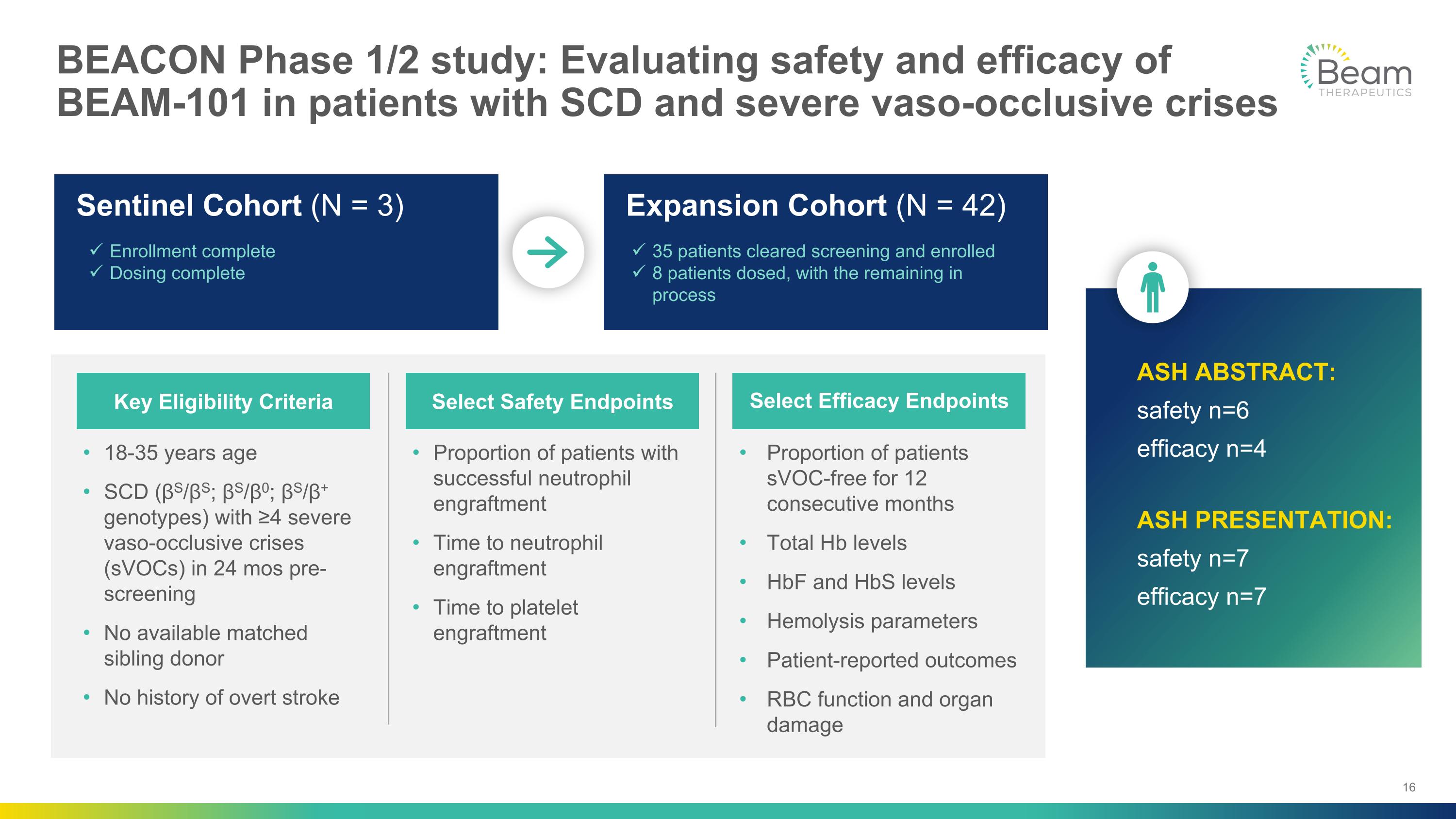
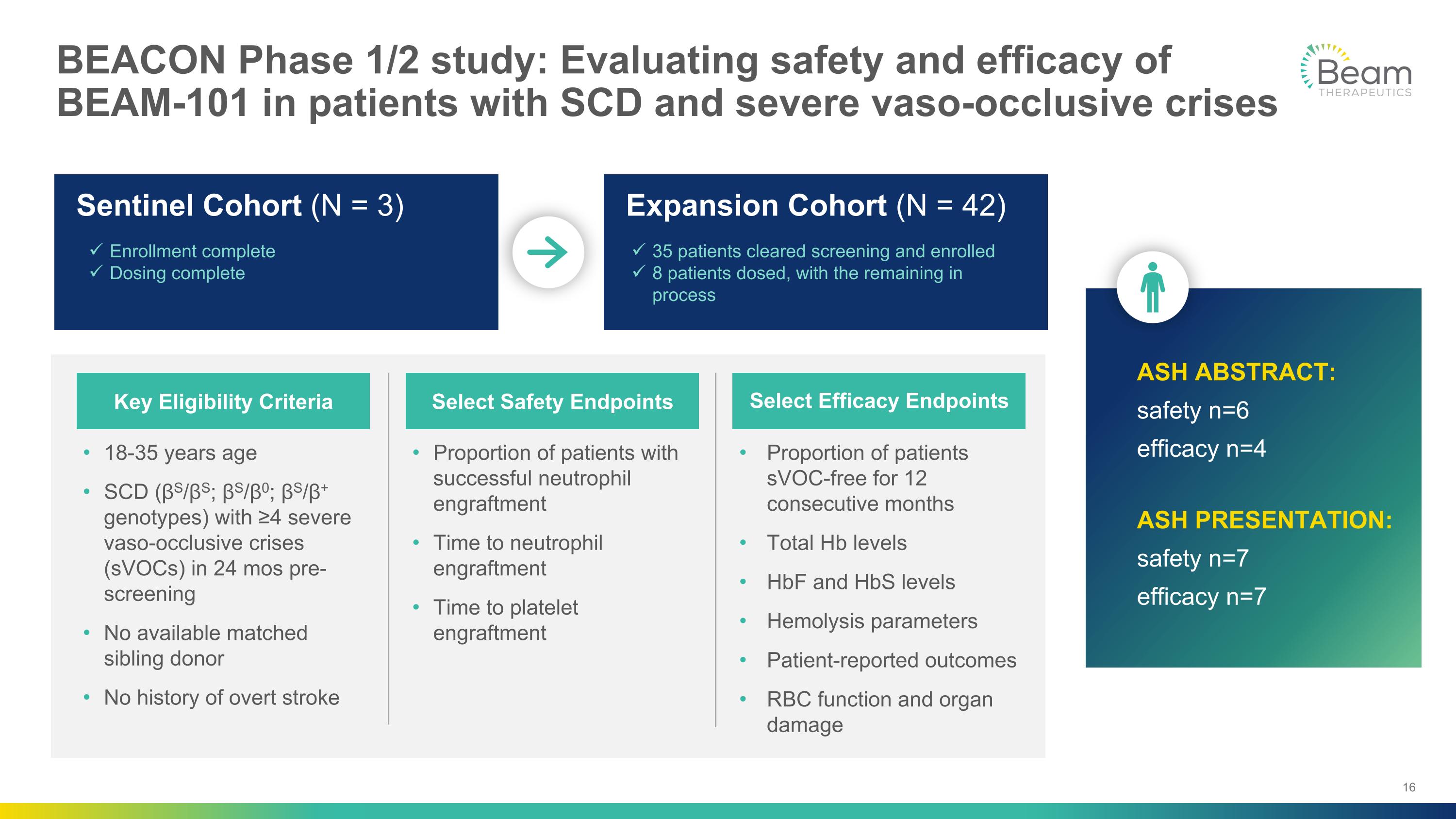
BEACON Phase 1/2 study: Evaluating safety and efficacy of BEAM-101 in patients with SCD and severe vaso-occlusive crises 18-35 years age SCD (βS/βS; βS/β0; βS/β+ genotypes) with ≥4 severe vaso-occlusive crises (sVOCs) in 24 mos pre-screening No available matched sibling donor No history of overt stroke Proportion of patients with successful neutrophil engraftment Time to neutrophil engraftment Time to platelet engraftment Proportion of patients sVOC-free for 12 consecutive months Total Hb levels HbF and HbS levels Hemolysis parameters Patient-reported outcomes RBC function and organ damage Key Eligibility Criteria Select Safety Endpoints Select Efficacy Endpoints Sentinel Cohort (N = 3) Expansion Cohort (N = 42) Enrollment complete Dosing complete 35 patients cleared screening and enrolled 8 patients dosed, with the remaining in process ASH ABSTRACT: safety n=6 efficacy n=4 ASH PRESENTATION: safety n=7 efficacy n=7
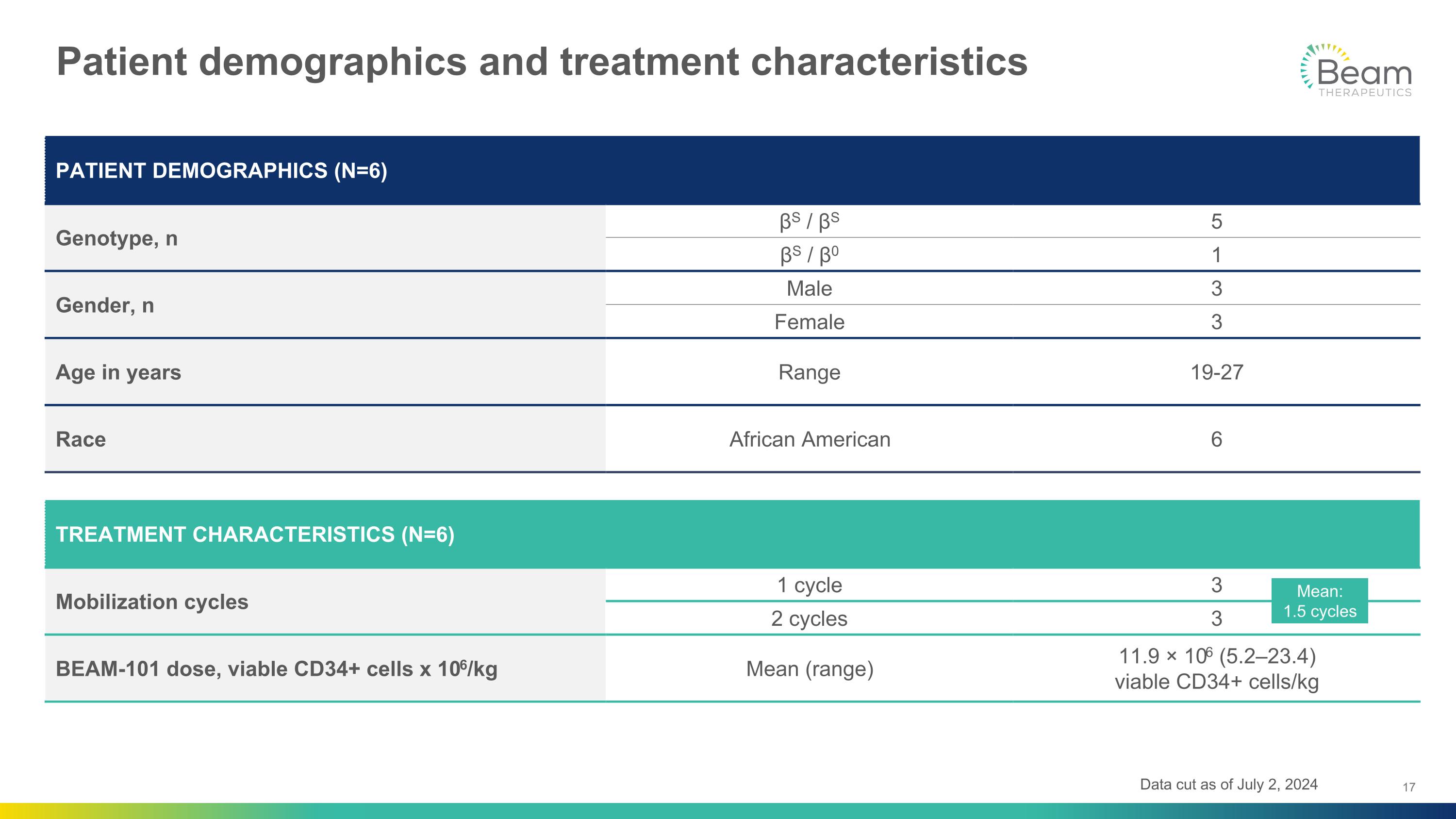
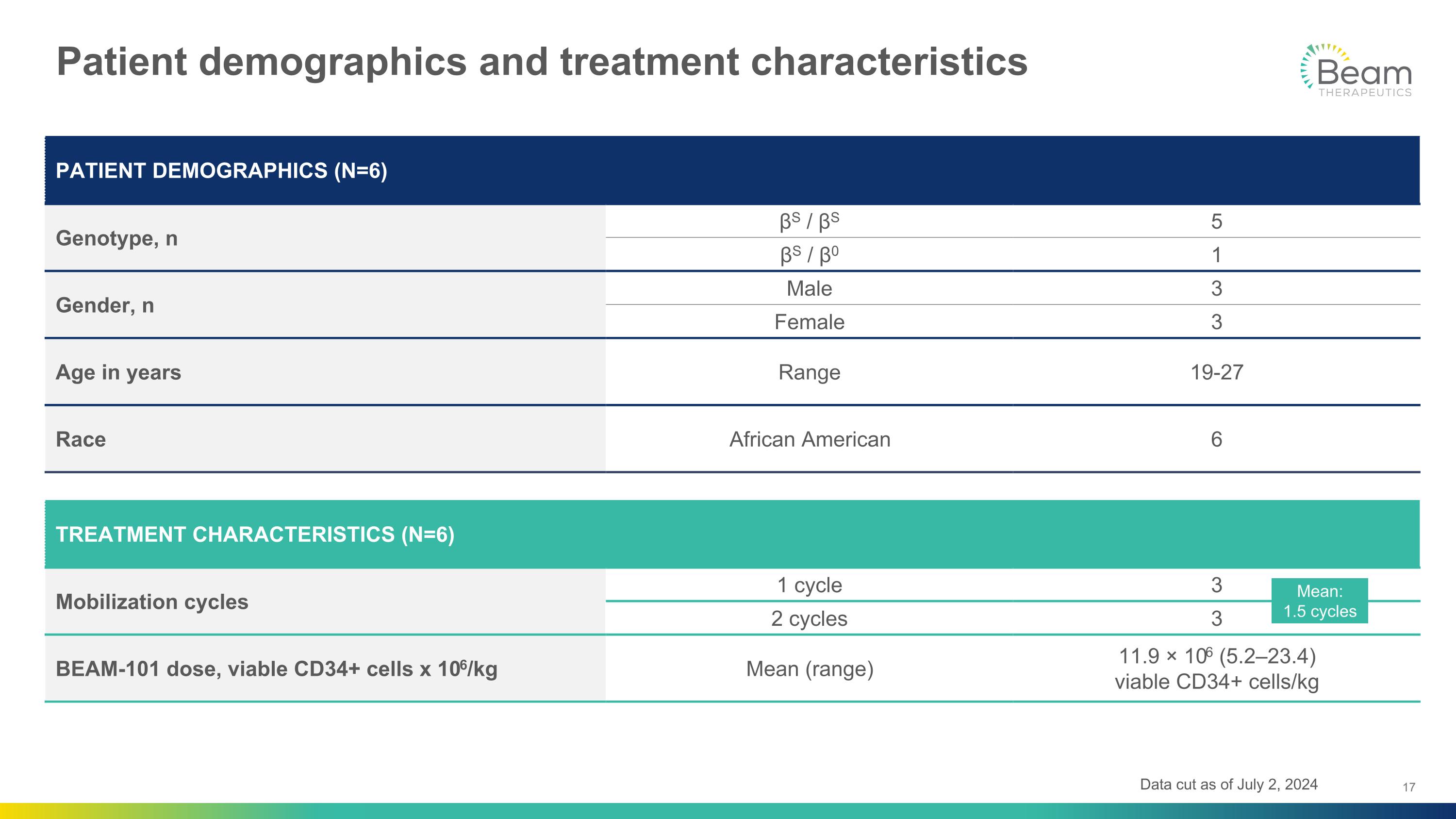
Patient demographics and treatment characteristics PATIENT DEMOGRAPHICS (N=6) Genotype, n βS / βS 5 βS / β0 1 Gender, n Male 3 Female 3 Age in years Range 19-27 Race African American 6 TREATMENT CHARACTERISTICS (N=6) Mobilization cycles 1 cycle 3 2 cycles 3 BEAM-101 dose, viable CD34+ cells x 106/kg Mean (range) 11.9 × 106 (5.2–23.4) �viable CD34+ cells/kg Mean:�1.5 cycles Data cut as of July 2, 2024

Preliminary safety data (N=6) Initial safety profile consistent with myeloablative conditioning with busulfan and autologous hematopoietic stem cell transplant (HSCT) One patient died due to respiratory failure likely related to busulfan conditioning 4 months after BEAM-101 infusion Unrelated to BEAM-101 as determined by investigator Case reviewed by Data Safety Monitoring Committee and FDA In all patients dosed, there were no ≥ Grade 3 adverse events (AEs) or serious AEs related to BEAM-101 Data cut as of July 2, 2024, with updated details regarding fatal event

Preliminary safety data: Time to engraftment (N=4*) Neutrophil Engraftment N=4 Platelet Engraftment N=4 Study Days after Drug Infusion Study Days after Drug Infusion 0 5 10 15 20 25 30 35 40 17 BEAM-101 Individual Patients BEAM-101 Median (Range) 20 BEAM-101 Individual Patients BEAM-101 Median (Range) 0 5 10 15 20 25 30 35 40 >90% allotransplant patients (peripheral blood stem cell) achieve neutrophil engraftment by Day 201 Approximately 60% of allotransplant patients (peripheral blood stem cell) achieve platelet engraftment by Day 302 Data cut as of July 2, 2024 *Data from patients with a follow-up period of one month or more 1Kawajiri A et al., Blood Cell Therapy, 2019. 2: 22-30 2Ramirez P et al., BMT 2011, 46:981-986
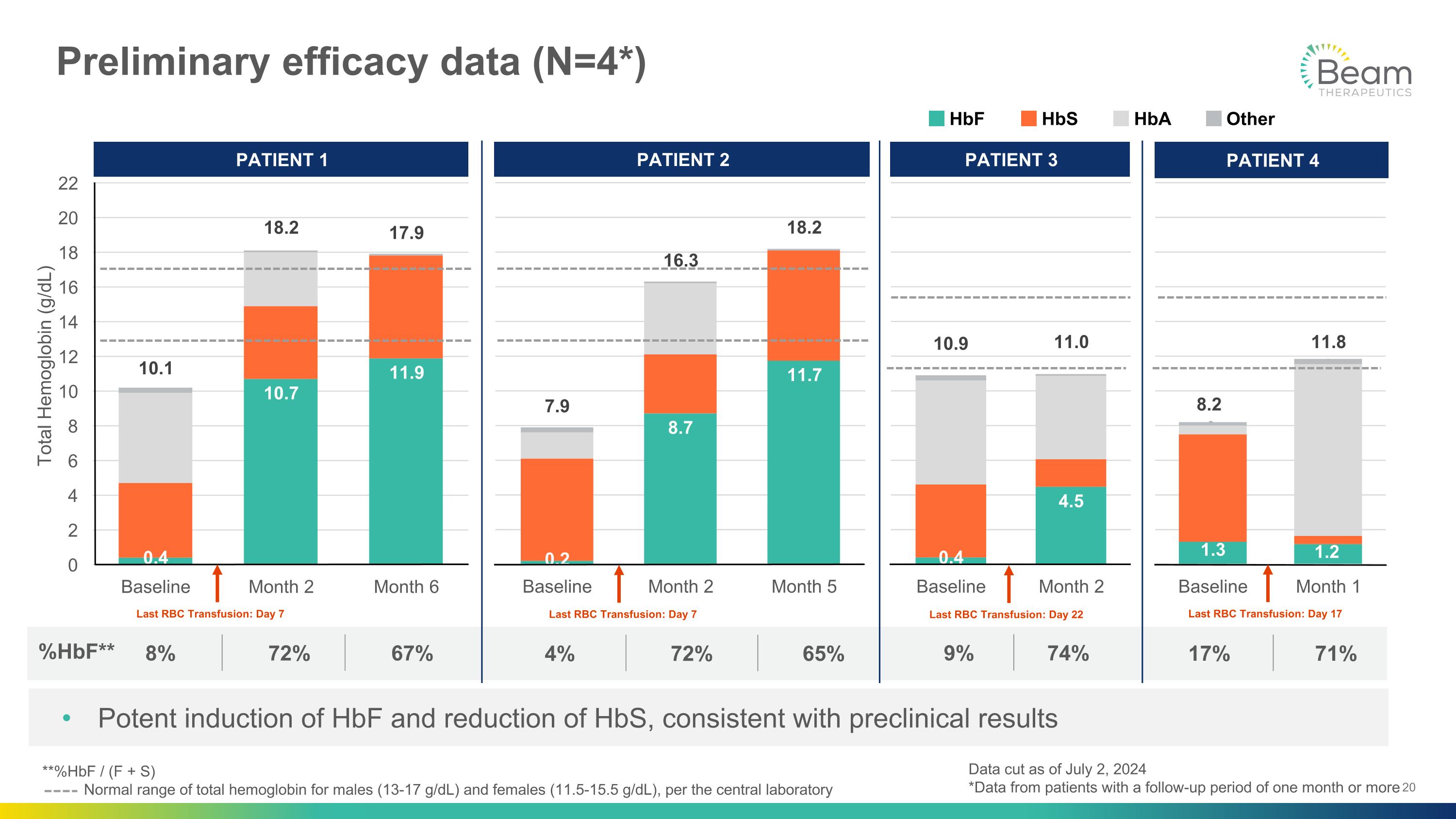
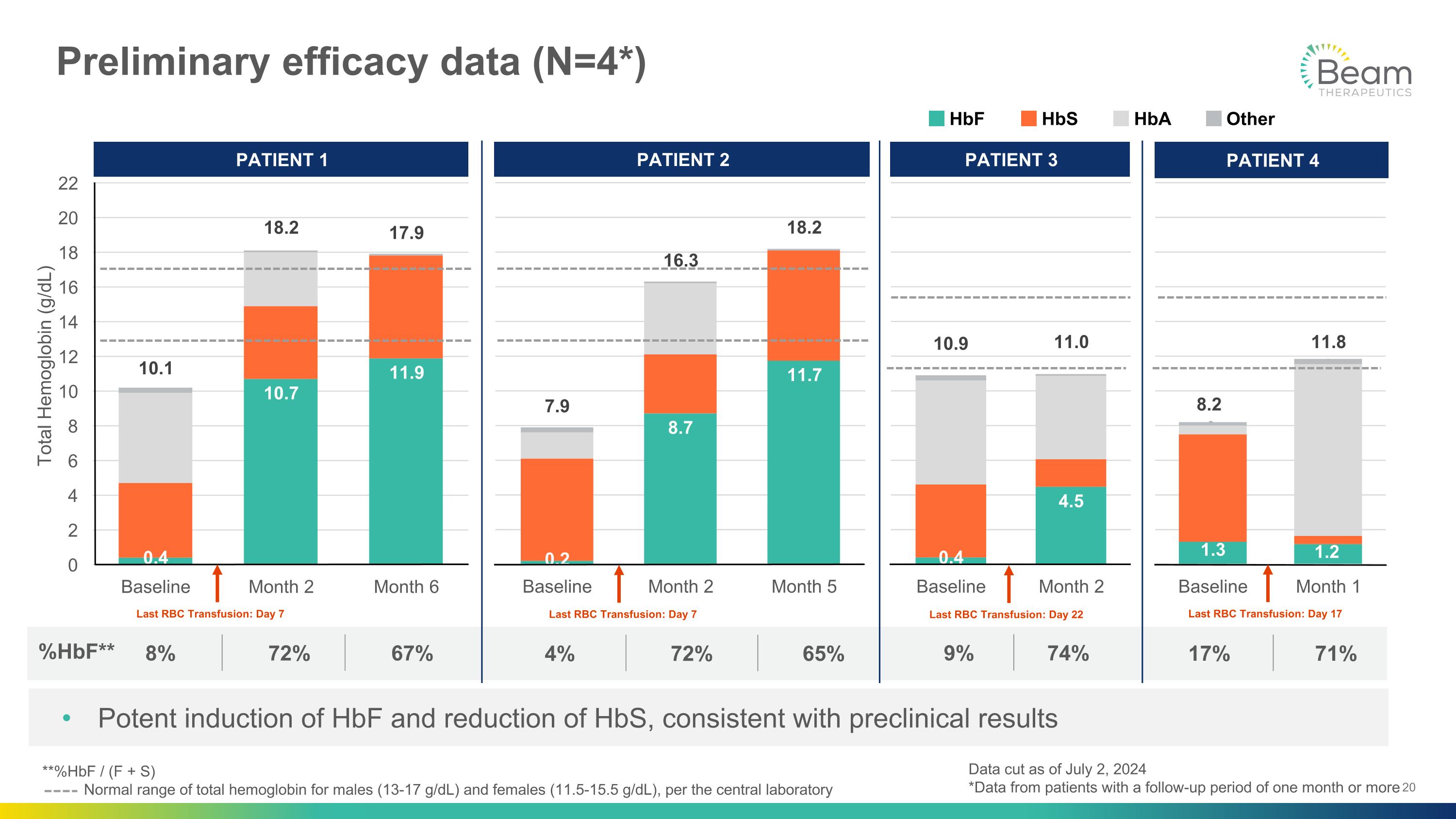
%HbF** Preliminary efficacy data (N=4*) 4% 72% 65% 9% 74% 17% 71% PATIENT 1 PATIENT 2 PATIENT 3 PATIENT 4 HbF HbS HbA Other Last RBC Transfusion: Day 7 Last RBC Transfusion: Day 7 Last RBC Transfusion: Day 17 Total Hemoglobin (g/dL) Last RBC Transfusion: Day 22 **%HbF / (F + S) Normal range of total hemoglobin for males (13-17 g/dL) and females (11.5-15.5 g/dL), per the central laboratory Potent induction of HbF and reduction of HbS, consistent with preclinical results 8% 72% 67% Data cut as of July 2, 2024 *Data from patients with a follow-up period of one month or more
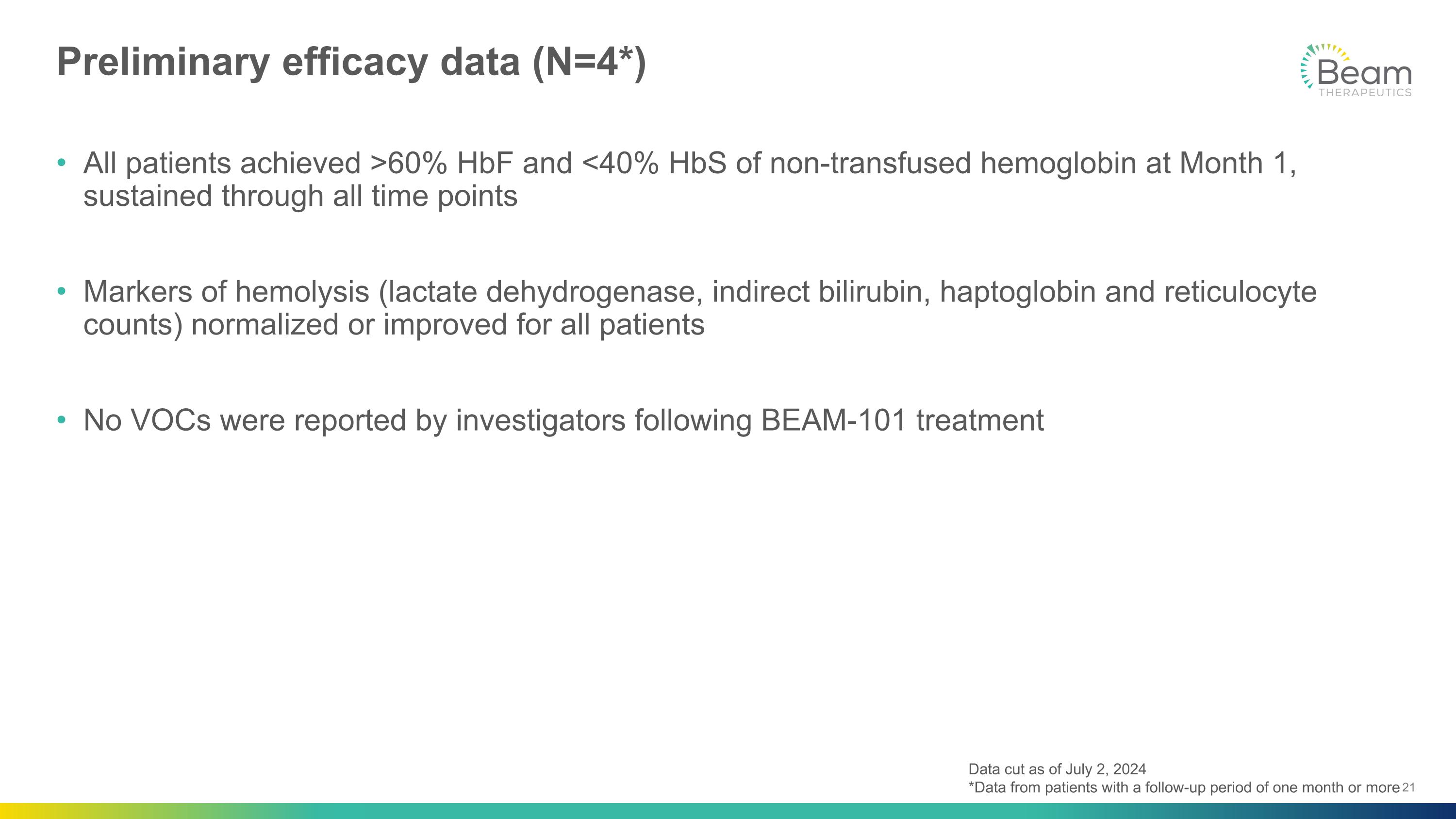
Preliminary efficacy data (N=4*) All patients achieved >60% HbF and <40% HbS of non-transfused hemoglobin at Month 1, sustained through all time points Markers of hemolysis (lactate dehydrogenase, indirect bilirubin, haptoglobin and reticulocyte counts) normalized or improved for all patients No VOCs were reported by investigators following BEAM-101 treatment Data cut as of July 2, 2024 *Data from patients with a follow-up period of one month or more

Exploratory red blood cell (RBC) function assays After BEAM-101 treatment: Nearly all RBCs were expressing HbF by Month 1 Nearly all RBCs expressing solely HbS were eliminated by Month 2 Data cut as of July 2, 2024 Duplex flow cytometry performed on untransfused RBCs
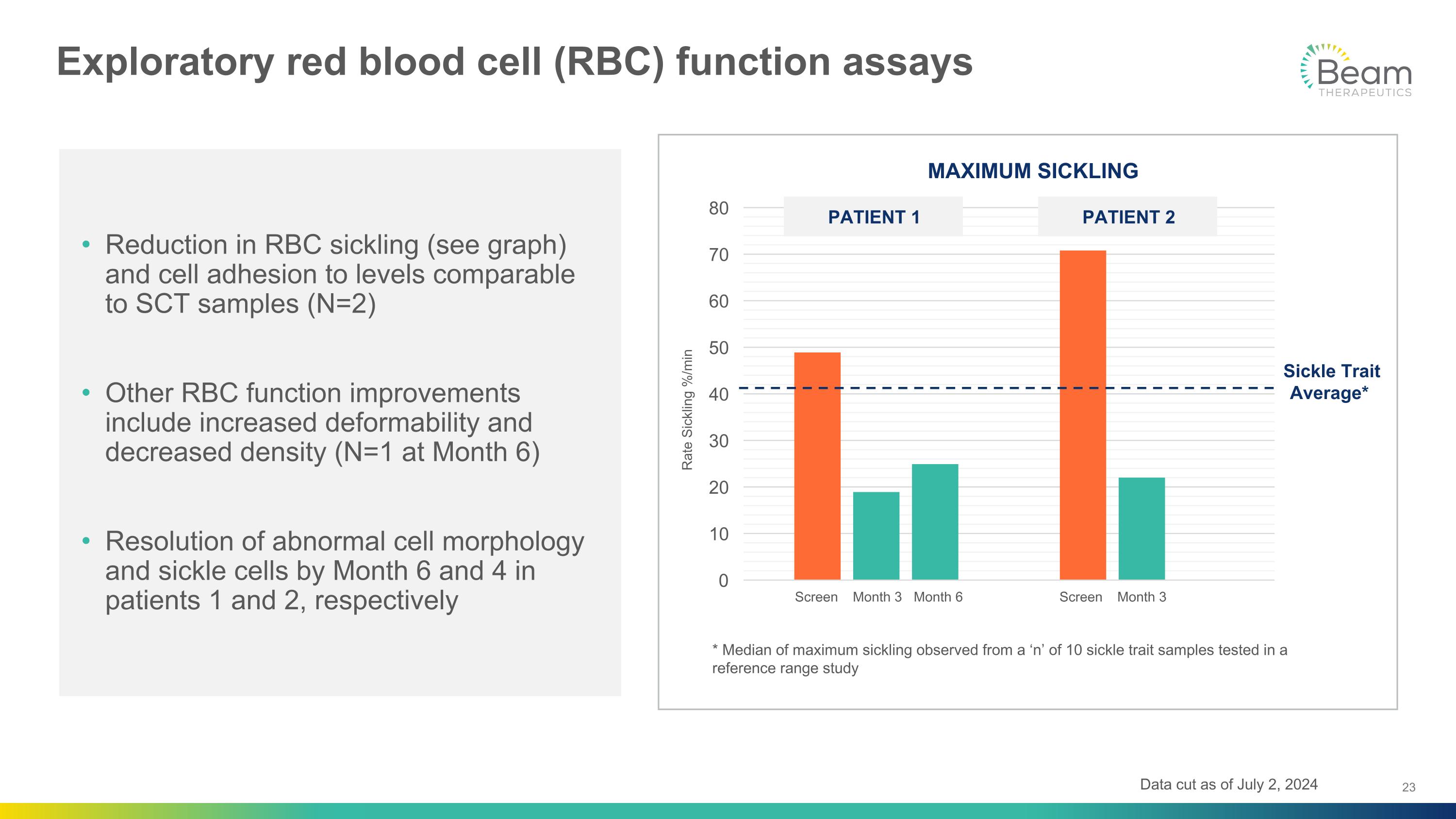
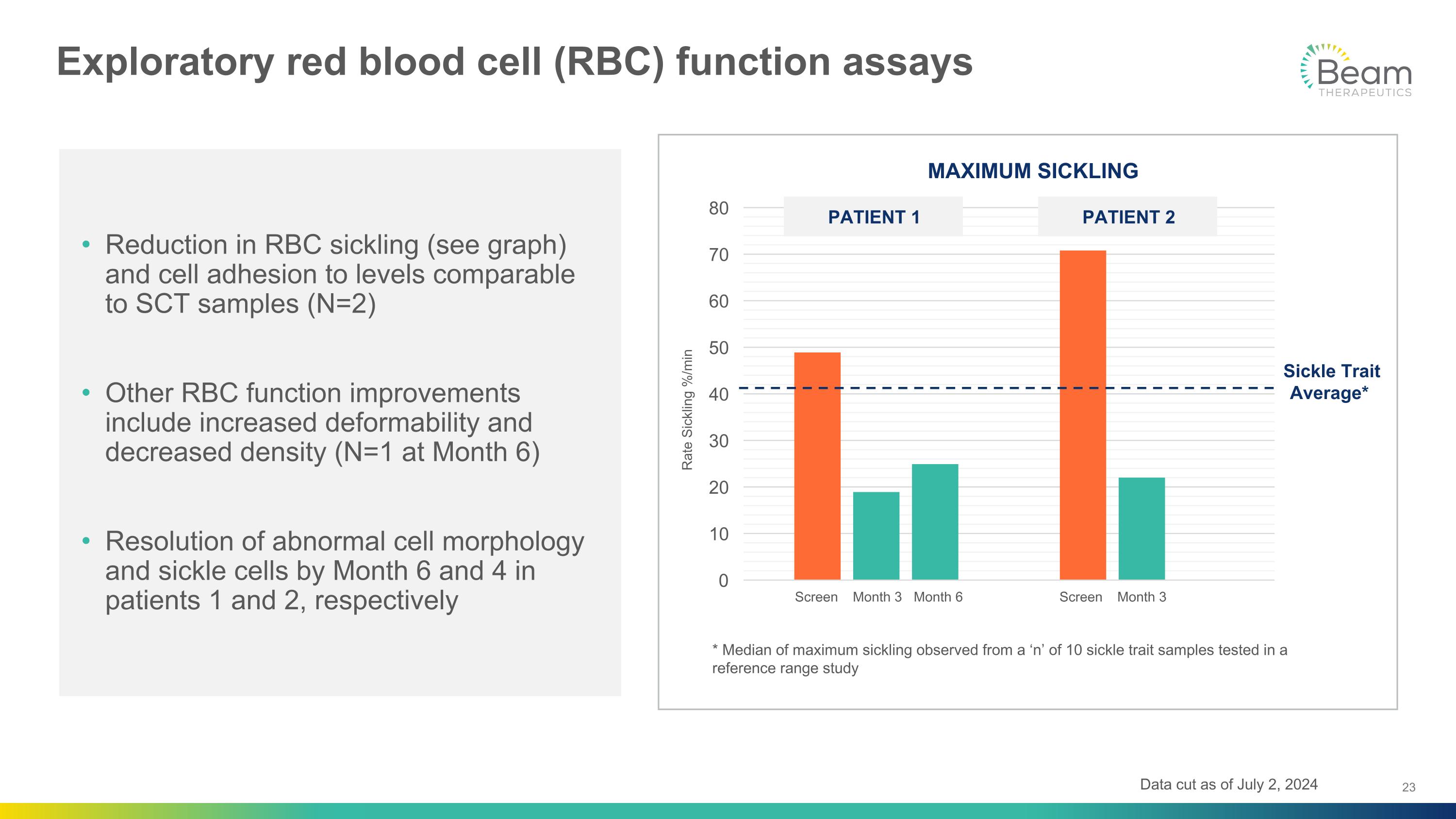
Exploratory red blood cell (RBC) function assays Sickle Trait�Average* Rate Sickling %/min * Median of maximum sickling observed from a ‘n’ of 10 sickle trait samples tested in a reference range study Reduction in RBC sickling (see graph) and cell adhesion to levels comparable to SCT samples (N=2) Other RBC function improvements include increased deformability and decreased density (N=1 at Month 6) Resolution of abnormal cell morphology and sickle cells by Month 6 and 4 in patients 1 and 2, respectively PATIENT 1 PATIENT 2 Screen Month 3 Month 6 Screen Month 3 Data cut as of July 2, 2024

Summary: Emerging BEACON data show potential for significant differentiation of base editing and BEAM-101 for SCD Neutrophil engraftment following busulfan conditioning occurred <20 days Potential to enable fewer hospital days Initial biomarker data demonstrate near elimination of RBCs solely expressing HbS and improved RBC function after BEAM-101 treatment Initial potent HbF induction and HbS reduction, consistent with preclinical �results: >60% HbF / <40% HbS Similar to sickle cell trait profile Presentation at ASH to include additional data with more patients �and longer follow-up Efficient cell collection process resulting in 1-2 cycles Potential to enable fewer hospital days Initial safety profile consistent with myeloablative conditioning with busulfan and autologous HSCT No SAEs related to BEAM-101

ESCAPE Program�Non-human Primate Data GIUSEPPE CIARAMELLA, PH.D., PRESIDENT

WAVE 3 ~100,000 Beam’s multi-wave strategy is focused on developing safer, more effective and more accessible treatments for patients with SCD WAVE 2 30-40,000 WAVE 1 ~10,000 ESCAPE: Multiple edits for non-genotoxic conditioning Designed to eliminate chemotherapy from ex vivo gene therapy and expand patient population with: Broader range of disease severity Broader age range Increased willingness-to-treat BEAM-101: Precise HbF upregulation Potentially best-in-class gene editing �Non-cutting, non-viral therapy with busulfan conditioning to address SCD with high vaso-occlusive crisis (VOC) burden In vivo: Base editing with HSC-targeted LNPs In vivo delivery would overcome need for transplantation, lower infrastructure requirements and unlock wider patient access and geographies Source: Internal Beam estimates Potential Eligible SCD Patient Population (U.S.)

WAVE 3 ~100,000 Beam’s multi-wave strategy is focused on developing safer, more effective and more accessible treatments for patients with SCD WAVE 2 30-40,000 ESCAPE: Multiple edits for non-genotoxic conditioning Designed to eliminate chemotherapy from ex vivo gene therapy and expand patient population with: Broader range of disease severity Broader age range Increased willingness-to-treat BEAM-101: Precise HbF upregulation Potentially best-in-class gene editing �Non-cutting, non-viral therapy with busulfan conditioning to address SCD with high vaso-occlusive crisis (VOC) burden In vivo: Base editing with HSC-targeted LNPs In vivo delivery would overcome need for transplantation, lower infrastructure requirements and unlock wider patient access and geographies Source: Internal Beam estimates Potential Eligible SCD Patient Population (U.S.) WAVE 2 30-40,000 ESCAPE: Multiple edits for non-genotoxic conditioning Designed to eliminate chemotherapy from ex vivo gene therapy and expand patient population with : Broader range of disease severity Broader age range Increased willingness-to-treat

ESCAPE technology designed to bring a paradigm shift to conditioning for the first time in nearly 70 years 1956 1st HSCT TBI conditioning AML 1959 Busulfan approved for CML 1984 1st SCD patient alloHSCT TBI/CP conditioning 1999 IV busulfan approval for HSCT conditioning 2014 1st Lovo-cel SCD patient dosed + busulfan conditioning 2019 1st Exa-cel SCD patient dosed + busulfan conditioning 2023 Exa-cel & Lovo-cel SCD approval in U.S. + busulfan conditioning 2024 ESCAPE development candidate 68 years of genotoxic conditioning: Promise of non-genotoxic conditioning Prevent acute and chronic toxicities Preserve fertility Potential to be outpatient Infertility Secondary malignancy Organ toxicities Infection complications Inpatient 2023 1st BEAM-101 SCD patient dosed + busulfan conditioning
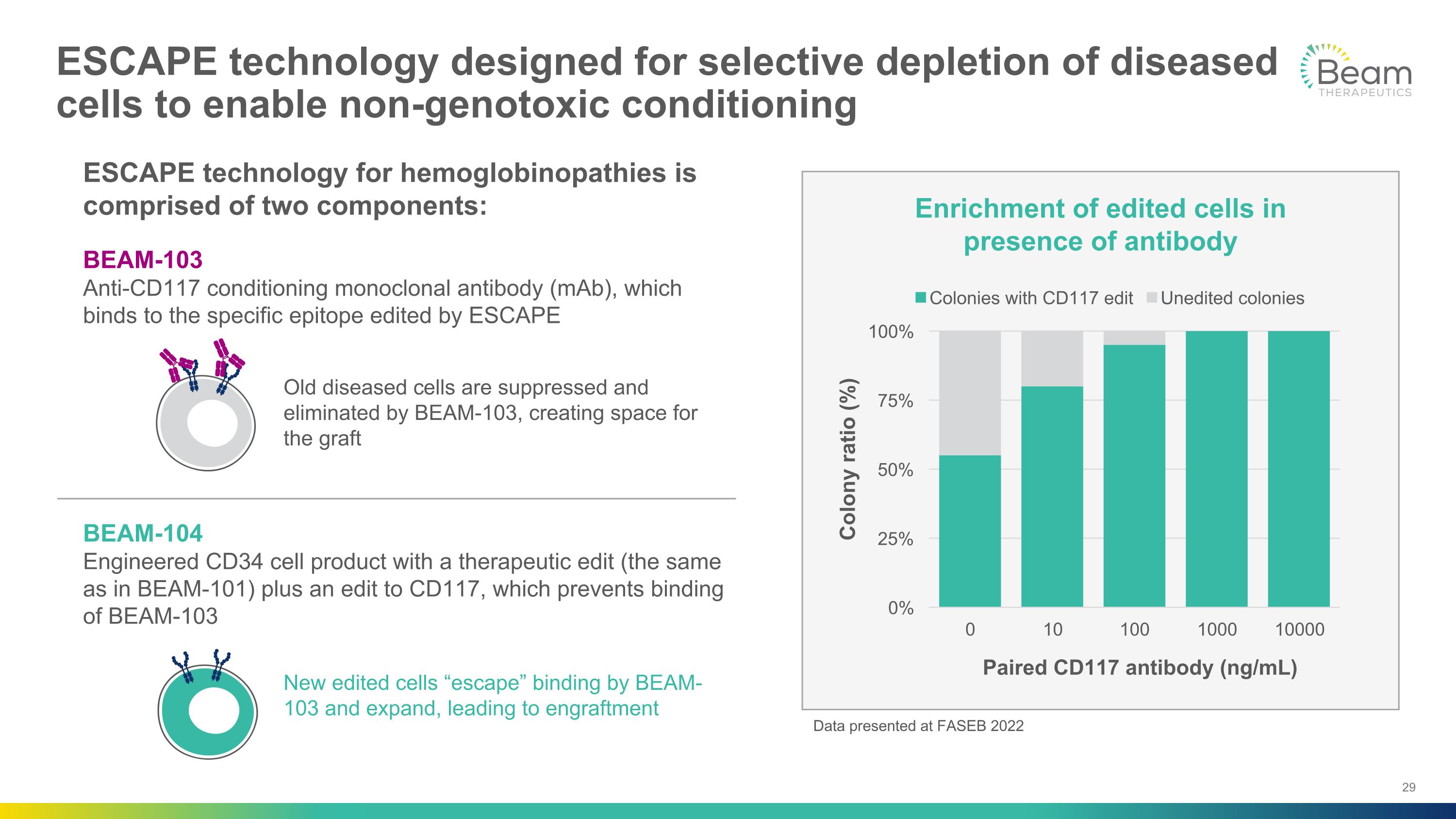
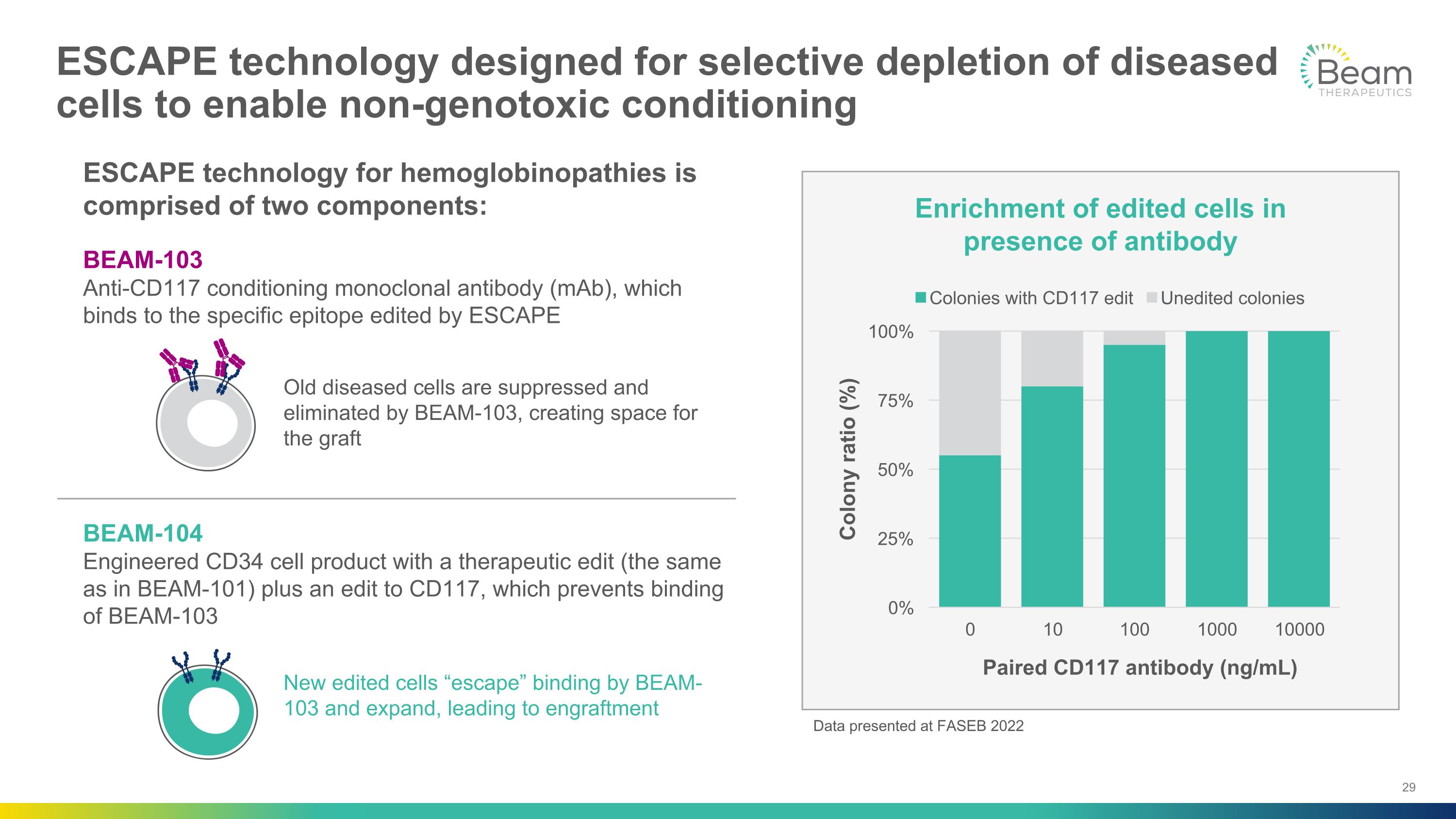
ESCAPE technology designed for selective depletion of diseased cells to enable non-genotoxic conditioning Enrichment of edited cells in presence of antibody Paired CD117 antibody (ng/mL) Colony ratio (%) Old diseased cells are suppressed and eliminated by BEAM-103, creating space for the graft New edited cells “escape” binding by BEAM-103 and expand, leading to engraftment BEAM-103 Anti-CD117 conditioning monoclonal antibody (mAb), which binds to the specific epitope edited by ESCAPE BEAM-104 Engineered CD34 cell product with a therapeutic edit (the same as in BEAM-101) plus an edit to CD117, which prevents binding of BEAM-103 ESCAPE technology for hemoglobinopathies is comprised of two components: Data presented at FASEB 2022

Assessing ESCAPE in a rigorous non-human primate (NHP) model of autologous transplant Proof-of-concept of non-genotoxic �antibody conditioning Can engraftment of HSCs be achieved without chemotherapy? Can a therapeutic level of fetal hemoglobin induction be achieved? Study design: Complete ex vivo gene editing �transplant with antibody conditioning ASH 2024

Long-term engraftment of base edited CD34 cells after antibody conditioning in NHPs led to high % F cells and HbF % Proof of concept of long-term engraftment after antibody conditioning, without chemotherapy, in NHPs % F-cells and HbF % at therapeutic thresholds comparable to gene therapy after 3-6 months mAb well tolerated – no myeloablation, no supportive care necessary Antibody dosed prior to infusion and monthly through week 35 *9 weeks for NHP #2 **34 weeks for NHP #2
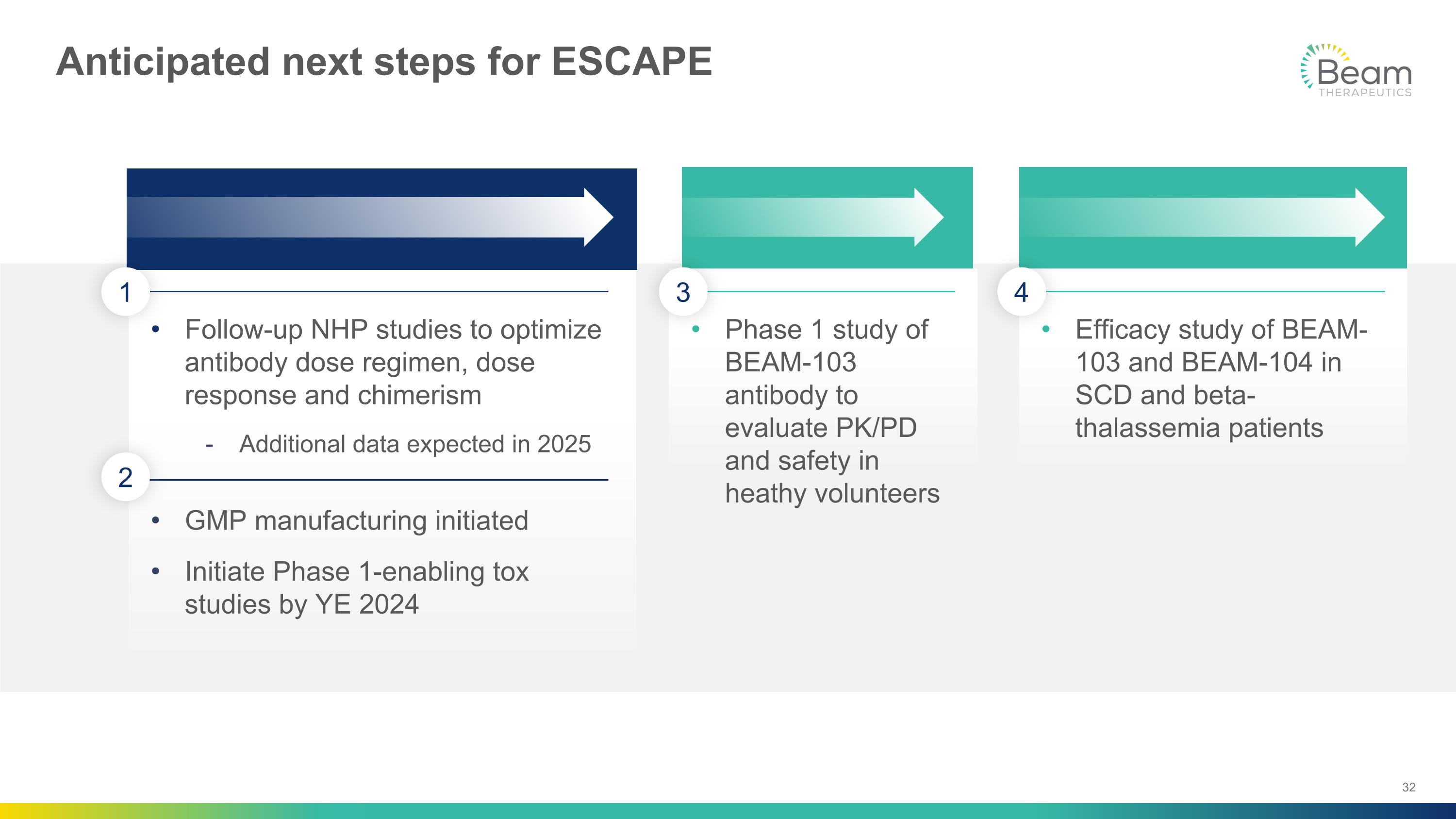
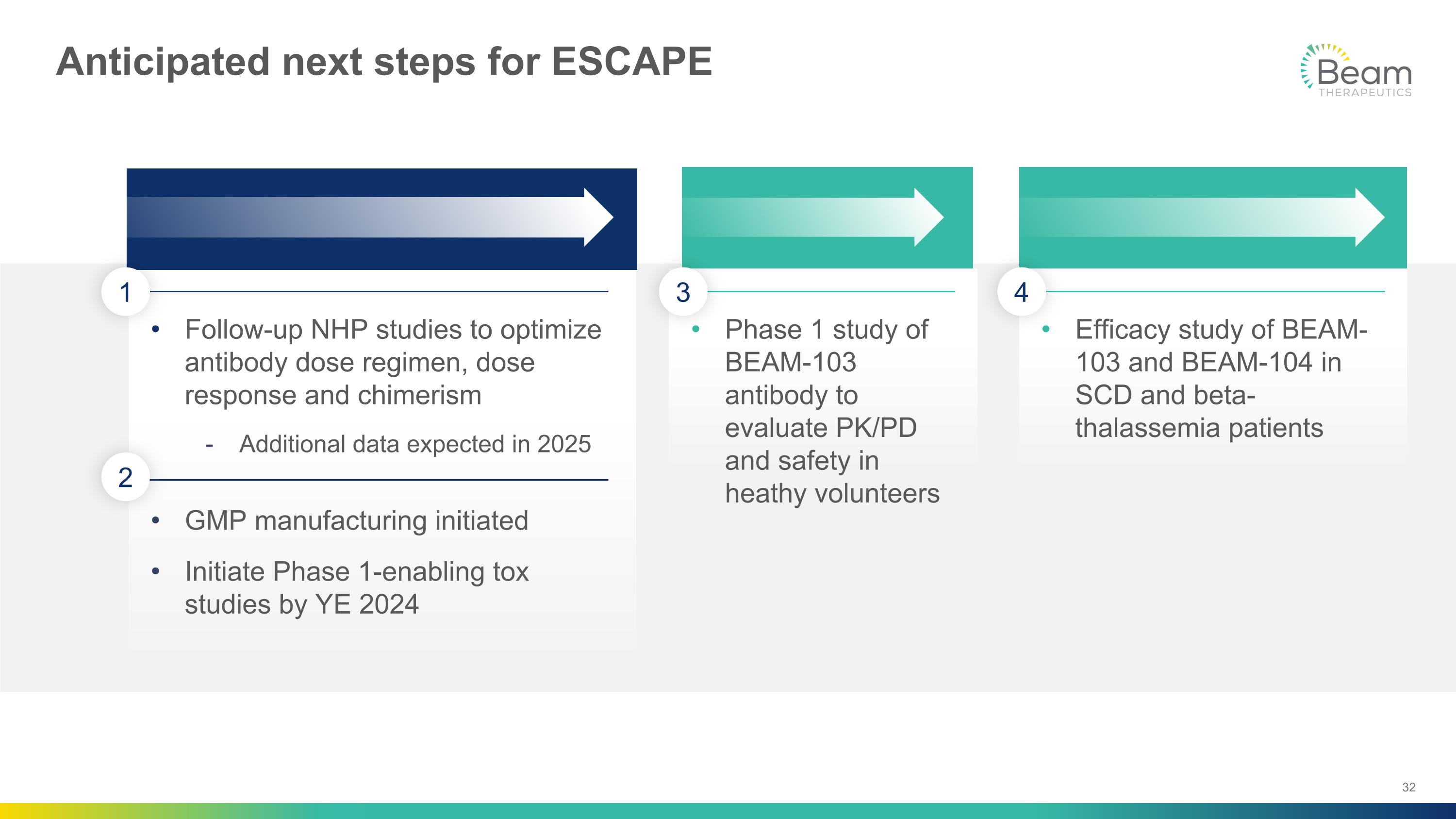
Follow-up NHP studies to optimize antibody dose regimen, dose response and chimerism Additional data expected in 2025 GMP manufacturing initiated Initiate Phase 1-enabling tox studies by YE 2024 Phase 1 study of BEAM-103 antibody to evaluate PK/PD and safety in heathy volunteers Efficacy study of BEAM-103 and BEAM-104 in SCD and beta-thalassemia patients Anticipated next steps for ESCAPE 2 1 3 4
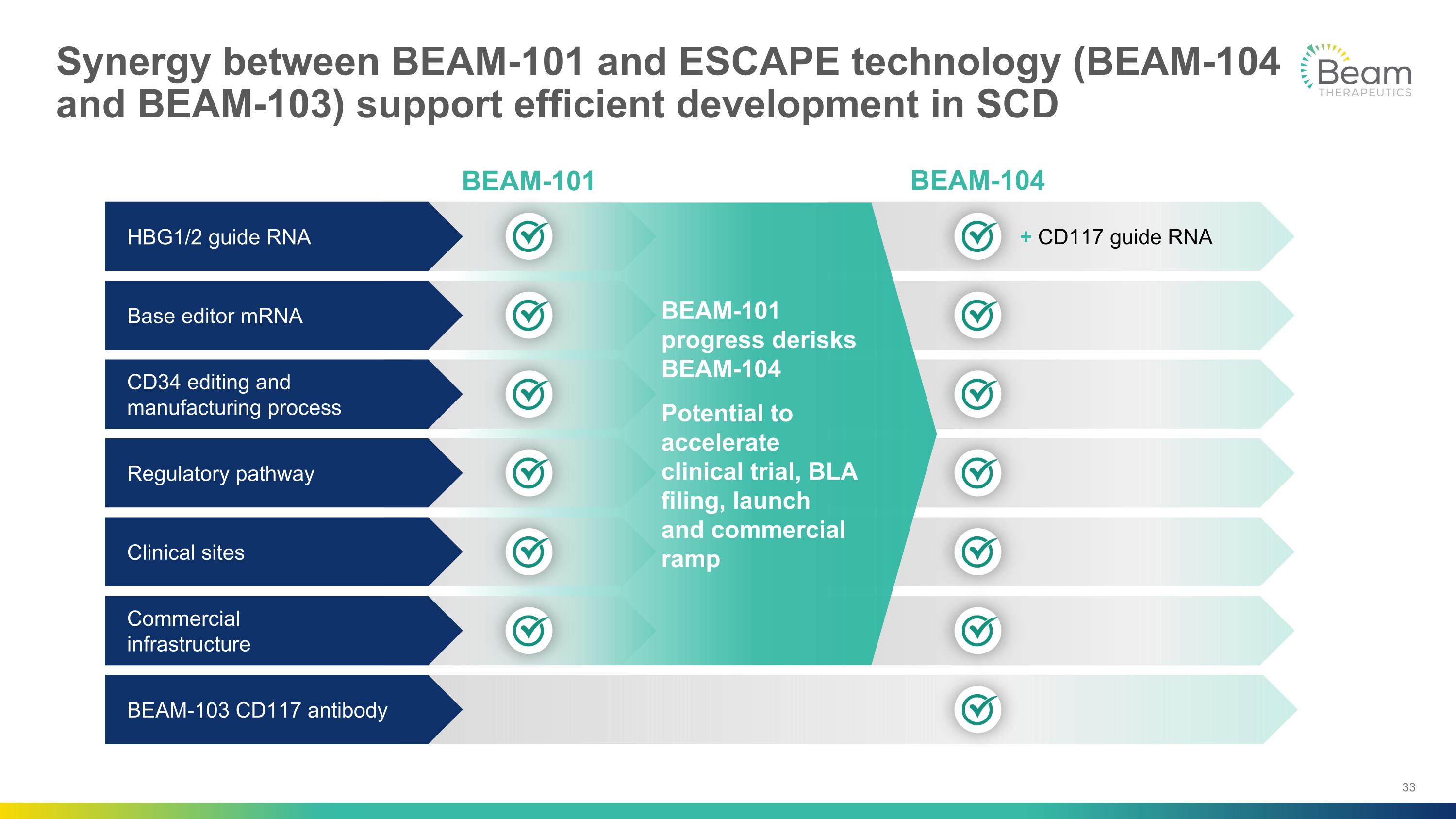
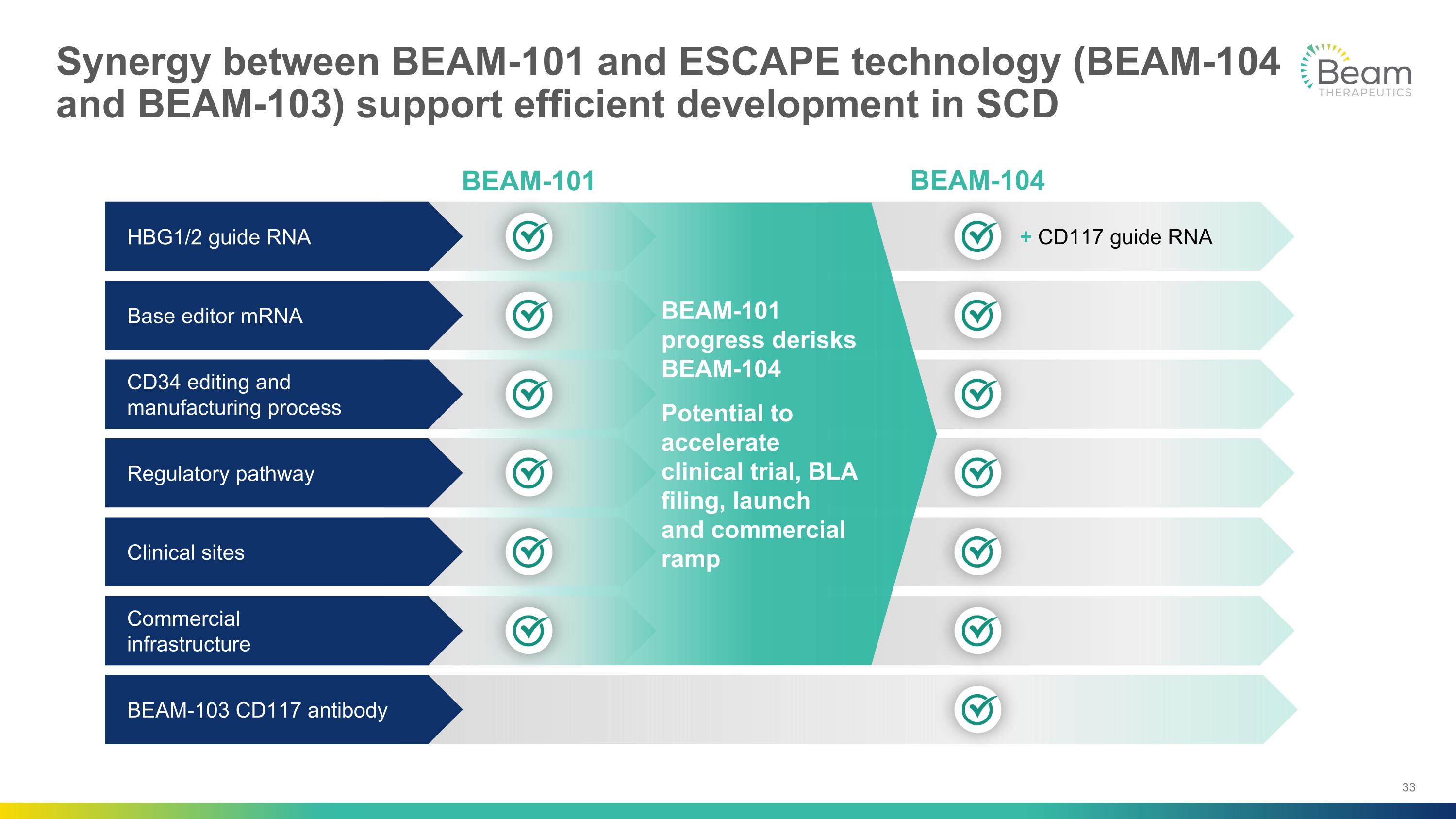
BEAM-101 progress derisks BEAM-104 Potential to accelerate clinical trial, BLA filing, launch and commercial ramp Synergy between BEAM-101 and ESCAPE technology (BEAM-104 and BEAM-103) support efficient development in SCD BEAM-101 BEAM-104 Regulatory pathway Clinical sites + CD117 guide RNA Commercial �infrastructure BEAM-103 CD117 antibody Base editor mRNA HBG1/2 guide RNA CD34 editing and manufacturing process

Significant step forward for Beam’s hematology vision and base editing platform Potentially differentiated clinical profile, comparable to sickle cell trait Potential to eliminate chemotherapy from transplant and expand the SCD market Technology validated, with strong translation from preclinical to clinical BEAM-101 in SCD ESCAPE NHP data Base editing

BEAM-201 Phase 1 Clinical Data MULTIPLEX BASE EDITING FOR CELL THERAPY

BEAM-201 abstract highlights: Data demonstrate proof of concept of 1st quad-edited, allogeneic CAR-T cell therapy Early evidence of clinical efficacy with CAR-T cell doses <200 million, as measured by CRi/CR in 2/3 patients Pharmacokinetic (PK) and safety data support continued Phase 1 dose exploration BEAM-201 safety profile consistent with underlying disease, lymphodepletion and AEs associated with CAR-T therapy Additional data will be presented at ASH Annual Meeting

Significant catalysts on the horizon for Beam Recent and Anticipated Catalysts BEAM-101 SCD Completed �sentinel dosing and initiated expansion Present initial clinical data �at ASH ESCAPE�SCD & BETA-THALASSEMIA Initiate Phase 1-enabling preclinical studies in 2024 Present NHP preclinical data�at ASH BEAM-302�AATD CTA cleared in the UK Initiate Phase �1/2 clinical trial Present initial data in 2025 BEAM-301�GSD1a Obtained U.S. IND clearance Dose first patient in Phase 1/2 study in early 2025 BEAM-201�T-ALL / T-LL Present initial clinical data �at ASH

Q&A